Assignment Diagnostic Method of Hemolytic anemia Assignment Sample
Introduction
The concept of Hemolytic anemia is considered as a type of disorder in the red blood cells of a human being which are mainly destroyed in a faster way than it is made in blood. It is known that the process of destruction is termed as hemolysis and addition with this, it is diagnosed that red blood cells help to carry oxygen to all the sections of the body.
Red blood cells have an important aim to carry oxygen from the lungs to the heart in the entire body of a human being. Bone marrow is considered as a responsible structure to make these kinds of blood cells. In a human being when the anemia is diagnosed, the process of testing is included with the measurement of levels of unconjugated bilirubin, reticulocyte and lactate haptoglobin, dehydrogenase. In this report the methods and limitations of the hematological practice in the concept of laboratory situation is made in terms of biological characteristics.
Discussion
Methods
Hemolytic anemia is the type of life-threatening disease that can harm the premature stage of the red blood cells. This disease is considered as an important part in the platform of differential diagnosis to macrocytic and normocytic anemia (Garden et al., 2019). There are various methods that are included in taking the initial laboratory tests to Hemolysis. The methods can be categorized in the form of:
| Tests | Hemolysis in Finding | Cause |
| Urinalysis | Positive in blood, Urobilinogen | It can proceed with the free hemoglobin and to the metabolites. |
| Unconjugated bilirubin | Increase in the level | It can increase the hemoglobin breakdown. |
| Reticulocyte count | Increase in the level | It has the marrow response to the anemia. |
| Peripheral blood smear | Abnorma;lity in the red blood cells | It is totally based on the main cause of anemia |
| Lactate dehydrogenase | Elevated | It can easily release from the lysis of the red blood cells |
| Haptoglobin | Decrease in the nature | It can find free hemoglobin |
Table 1: Initial Test to the Hemolysis
(Source: https://www.aafp.org/afp/2018/0915/p354.html)
Even if there are no visible RBCs on microscopy, a urine test for hemoglobinuria in hemolytic anaemia may be positive. Hemolysis is confirmed by the presence of reticulocytosis, elevated lactate dehydrogenase levels, elevated unconjugated bilirubin levels, and decreased haptoglobin levels. The lack of these discoveries should lead to a search for alternative causes (Jäger et al., 2020). After hemolysis has been confirmed, supportive treatment should be started as needed.
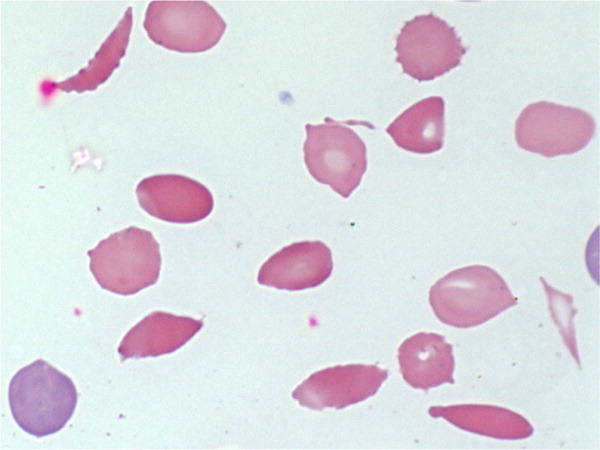
Figure 1: Giemsa-Wright peripheral smear blood
(Source: https://www.aafp.org/afp/2018/0915/p354.html)
A study of the medical history and symptoms is frequently the first step in diagnosing hemolytic anemia. Your doctor will look for pale or yellowed skin during the physical exam. They may also gently press on various parts of your abdomen to feel tenderness, which might also demonstrate an augmented digestive system or gallbladder. Unconjugated bilirubin levels, Lactate dehydrogenase, reticulocyte, haptoglobin and, as well as urinalysis, should all be measured when anemia is suspected.
Limitation
The hemolytic anemia diagnostic workup and laboratory technique relies on rigorous step-by-step analysis that encompasses red blood cell shape, haematological parameters including higher erythrocytes frequency, and clinical symptoms of hemolytic anemias. Genetic screening is suggested if traditional laboratory studies fail to discover the underlying cause of hemolysis. If thalassemias/ hemoglobinopathies are present, “Sanger sequencing” combined with traditional screening is the most economical technique to determine the genetically determined reasons (Veterinary et al., 2019). However, because hemolytic anemia are complex and heterogeneous illnesses, succeeding batch processing screenings quickly will become an effective technique to figure out the explanations when frequent causes have indeed been ruled out.
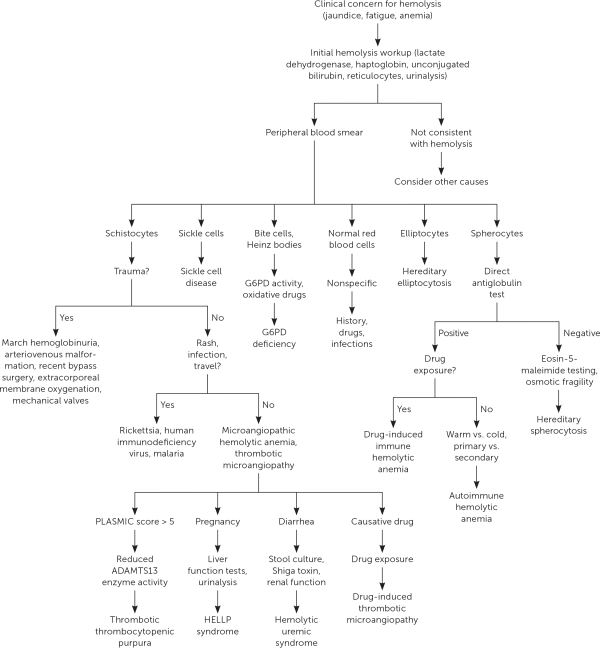
Figure 2: Evaluation to the suspected hemolysis
(Source: https://www.aafp.org/afp/2018/0915/p354.html)
Laboratory tests are mainly resulted to form or provide confirmation to the process of hemolysis that can include reticulocytosis that can increase lactate dehydrogenase which can decrease haptoglobin and increased unconjugated bilirubin. Several hemolytic anemia can also cause shocks, abdomen, pain in the back, fever and chills (Huisjes et al., 2018). This types of anemia is not controlled or treated which can lead with the “serious complications” like arrhythmias, which is known as the “irregular heart rhythms” and cardiomyopathy that can increase heart rates and also increase the measurement of shape of heart which can grow larger than the normal. It can also lead to heart failure. The risks are included with the category of:
- Family history to the hemolytic disease
- Disease if collagen vascular like a systematic way of lupus erythematosus
- Cancers like leukemia
- Infection like atypical pneumonia, mononucleosis and viral infections.
These kinds of methods to diagnose anemia can easily cause various health problems like extreme fatigue. Various methods to diagnose anemia makes someone so tired that he or she can not complete various tasks. It can also cause pregnancy complications to the human being. Untimely annihilation of RBCs can happen intracellularly or extracellularly in the reticuloendothelial framework, albeit the last option is more normal (Barcellini et al., 2020). The essential extravascular instrument is sequestration and phagocytosis because of helpless RBC deformability.
Relevance of methods
Various treatment options for the hemolytic anemia help to differ depending on various reasons of the anemia, health, age, severity to the conditions and the tolerance of the “certain” medications. As it can be seen that there are various way to diagnose hemolytic anemia but in specific ways also it can be treated which are considered as:
-
Surgery
In various cases spleens are needed to be destroyed or removed. That is why the spleen is the condition where the red blood cells are destructed. The process of removing the existing spleen can also reduce the way of how fast the red blood cells are destroyed (Durani et al., 2018). The process is also used as various options in the platform of immune hemolysis which can respond to immunosuppressant’s or corticosteroids.
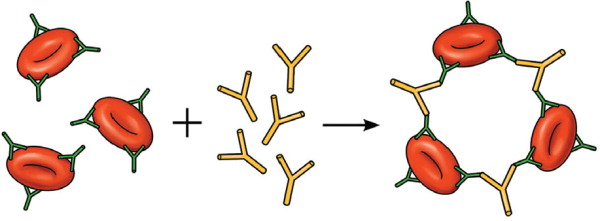
Figure 3: Direct Antiglobulin Test
(Source: https://www.aafp.org/afp/2018/0915/p354.html)
-
Corticosteroids
It can helps to reduce the immune system and helps to prevent red blood vcells to being destructed. Various immunosuppressant’s can also be used for achieving the exact goal.
-
Red blood cell transfusion
The concept of transfusion of red blood cells is known as the form of quick increase to the count of red blood cells and helps to replace or destroy the “red blood cells” with the new ones.
On the other hand hemolysis inducing agents have various mechanism to the drugs which can be categorized as:
| Mechanisms | Drugs |
| Oxidation | Rifampin, ribavirin, recreational nitrates, primaquine, phenazopyridine, nitrofurantoin, Dapsone. |
| Induced drugs hemolytic anemia | sulfamethoxazole/ trimethoprim, Prograf or tacrolimus, Zocor or simvastatin quinine, Seroquel or quetiapine, nitrofurantoin, Flagyl or metronidazole, mefloquine, interferon, ibuprofen, Sandimmune, cyclosporine, cocaine, Plavix or clopidogrel, chemotherapy, Wellbutrin or bupropion, Ecstasy or 3,4-methylenedioxymethamphetamine. |
Table 2: Hemolysis-Inducing Agents
(Source: https://www.aafp.org/afp/2018/0915/p354.html)
MAHA or Microangiopathic hemolytic anemia is considered as a descriptive term which can occur in the times of RBCs fragment and this can be resulted in the schistocytes which are visible on the “peripheral bloodsphere”.
Application of the method
Enzymopathies bring about hemolysis because of overpowering oxidative pressure or diminished energy creation. In safe interceded hemolytic iron deficiency, antibodies tie with the RBCs, bringing about phagocytosis or supplement intervened obliteration. The outward non immune causes incorporate microangiopathic hemolytic pallor (MAHA), diseases, direct injury, and medication actuated hemolysis, among others (Swann et al., 2019). Various diagnosis process of hemolysis can be categorized in the form of:
| Type/Class | Mechanism | Disease | Site | Treatment | Laboratory Test |
| Membranopathy | Paroxysmal hemoglobinuria nocturnal elliptocytosis, hereditary spherocytosis. | Trapping | Extravascular | Fragalitic test of osmotic pressure, binding if eosin-5-maleimide | Splenectomy eculizumab |
| Alloimmune | The process of the method to transfusion reactions and hemolytic disease to trghe newborn and the fetus. | Complement, phagocytosis, trapping | Intravascular | DAT Neonatal | Supportive Halt transfusion. |
| Drug induced | drug-induced immune hemolytic anemia, Drug-induced thrombotic microangiopathy, and oxidative hemolysis. | Fragmentation, phagocytosis, and Direct toxin. | Intravascular or extravascular | DAT Neonatal | Treatment to the other disease, avoidance of steroids. |
| Hemoglobinopathy | hemoglobin defects, thalassemias, Sickle cell disease. | Trapping | Extravascular | Electrophoresis hemoglobin | Disease related treatment |
Table 3: Various diagnosis process
(Source: https://www.healthline.com/health/sickle-cell-anemia)
It can be seen hat6 when hemolysis is suspected then the history of the diseases should be included with the medical diagnoses, family or personal history to the hemolytic anemia, medications and the “complete review” of the main systems (Deng et al., 2020). On the other hand, the concept of physical examinations should also be focused on the identified associated conditions like malignancies or infections.
At the point when iron deficiency is recognized, trying ought to incorporate estimation of lactate dehydrogenase, haptoglobin, reticulocyte, and unconjugated bilirubin levels, just as urinalysis. Spherocytes are brought about by film deficiencies or rehashed little layer evacuations by macrophages (Moraes et al., 2019). Spherocytosis isn’t analytic for hemolytic paleness on the grounds that both inherited spherocytosis and resistant etiologies.
Conclusion
In the end one might say that the course of annihilation is named as hemolysis and expansion with this, it is analyzed that red platelets help to convey oxygen to every one of the segments of the body.
Red platelets have a significant expectation to convey oxygen from the lungs to the heart in the whole body of a person. Bone marrow is considered as a capable design to make these sorts of platelets.
In a person when the pallor is analyzed, the most common way of testing is incorporated with the estimation of levels of unconjugated bilirubin, reticulocyte and lactate haptoglobin, dehydrogenase. In this report the strategies and limits of the hematological practice in the idea of lab circumstance is made as far as organic attributes.
Reference List
Journals
Barcellini, W., Zaninoni, A., Giannotta, J.A. and Fattizzo, B., 2020. New Insights in Autoimmune Hemolytic Anemia: From Pathogenesis to Therapy. Journal of clinical Medicine, 9(12), p.3859.
Deng, J., Zhou, F., Wong, C.Y., Huang, E. and Zheng, E., 2020. Efficacy of therapeutic plasma exchange for treatment of autoimmune hemolytic anemia: a systematic review and meta‐analysis of randomized controlled trials. Journal of clinical apheresis, 35(4), pp.294-306.
Durani, U., Go, R.S. and Kay, N.E., 2018. Immune-mediated hemolytic anemia and thrombocytopenia in clonal B-cell disorders: a review. Clin Adv Hematol Oncol, 16(10), pp.670-676.
Garden, O.A., Kidd, L., Mexas, A.M., Chang, Y.M., Jeffery, U., Blois, S.L., Fogle, J.E., MacNeill, A.L., Lubas, G., Birkenheuer, A. and Buoncompagni, S., 2019. ACVIM consensus statement on the diagnosis of immune‐mediated hemolytic anemia in dogs and cats. Journal of veterinary internal medicine, 33(2), pp.313-334.
Huisjes, R., van Solinge, W.W., Levin, M.D., van Wijk, R. and Riedl, J.A., 2018. Digital microscopy as a screening tool for the diagnosis of hereditary hemolytic anemia. International journal of laboratory hematology, 40(2), pp.159-168.
Jäger, U., Barcellini, W., Broome, C.M., Gertz, M.A., Hill, A., Hill, Q.A., Jilma, B., Kuter, D.J., Michel, M., Montillo, M. and Röth, A., 2020. Diagnosis and treatment of autoimmune hemolytic anemia in adults: Recommendations from the First International Consensus Meeting. Blood reviews, 41, p.100648.
Moraes, M.L., Lima, L.R., Vicentini-Oliveira, J.C., de Souza, A.V.G., Oliveira, O.N., Deffune, E. and Ribeiro, S.J., 2019. Immunosensor for the Diagnostics of Autoimmune Hemolytic Anemia (AIHA) Based on Immobilization of a Monoclonal Antibody on a Layer of Silk Fibroin. Journal of nanoscience and nanotechnology, 19(7), pp.3772-3776.
Swann, J.W., Garden, O.A., Fellman, C.L., Glanemann, B., Goggs, R., LeVine, D.N., Mackin, A.J. and Whitley, N.T., 2019. ACVIM consensus statement on the treatment of immune‐mediated hemolytic anemia in dogs. Journal of veterinary internal medicine, 33(3), pp.1141-1172.
Veterinary and Comparative Clinical Immunology Society Diagnostic Task Force, MacNeill, A.L., Dandrieux, J., Lubas, G., Seelig, D. and Szladovits, B., 2019. The utility of diagnostic tests for immune‐mediated hemolytic anemia. Veterinary Clinical Pathology, 48, pp.7-16.
………………………………………………………………………………………………………………………..
Know more about UniqueSubmission’s other writing services:

