Assignment Sample on Lab Report in Pharmacology
Introduction
A chronic metabolic disorder, Diabetes Mellitus affects millions of people globally. This disorder poses a consequential global health burden. Due to this chronic disease blood glucose level is elevated for either insufficient production of insulin in the pancreas or the individual body’s inability to utilize insulin effectively. With the prevalence of diabetes increasing steadily, there is an emergency need for innovative therapeutic approaches to prevent and reduce the associated complications. Compound 2 is a promising novel compound that has emerged as a potential prevention of diabetes. Developing through advanced research compound 2 represents an advanced drug that fights against diabetes. The Compound 2 mechanism actions are numerous and highly specific that target the key pathways that are associated with diabetes development. The primary mode of action is increasing insulin sensitivity in the target tissue which allows cells to respond to insulin and helps to blood glucose levels effectively. Also, Compound 2 demonstrated the capability to promote the function of beta cells and safeguard the insulin-producing cells in the pancreas from degeneration and damage.
Method
Diabetes mellitus is a chronic type metabolic disease, due to this blood glucose level rise that resulting from insulin resistance or secretion of insulin in insufficient amounts. “Glucagon-like peptide 1 (GLP-1)” is a crucial hormone that is associated with the metabolism of glucose and this “plays an important role in the secretion of insulin”, slowing gastric emptying and also suppressing appetite. For its significance in diabetes management. GLP-1 receptor and GLP-1 analogue have emerged as therapeutic agents for treating type 2 diabetes (Babu, et al. 2021). The development of drug testing rigorously involved assessing pharmacodynamics and pharmacokinetic characteristics, efficacy and safety. This component tests for drug development of diabetes and focuses on different essential experimental methods and considerations also.
GLP-1 peptide synthesis:
The initial step conducting GLP-1 peptide testing which is associated with the GLP-1 peptide synthesis itself. This compound is a 30-amino-acid peptide hormone. In these components, synthetic analogues are designed that provide stability and this has longer half-lives. Here use Solid phase peptide synthesis (SPSS) for preparation of GLP-1 peptides (Batista, et al. 2019). This scientific process is associated with the sequential addition of protected amino acids for the solid resin support. This substance is then cleaved and deprotected to yield the desired peptide for the drug.
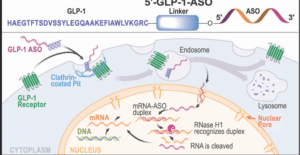
Figure 1: GLP-1 peptide synthesis
(Source: pubs.acs.org)
In vitro GLP-1 stability testing:
To proceed with the vivo studies this is very essential to the stability assess of the GLP-1 synthesized that analogue under the physiological condition. The stability of the study is conducted to determine the susceptibility of the peptide to the dipeptidyl peptidase-4 enzymatic degradation. This degrades rapidly endogenous for the GLP-1 (Chia and Egan, 2020). The analogue’s stability is analysed in the stimulation of intestinal and gastric fluids that basically mimic the gastrointestinal environment.
GLP-1 receptor binding assays
To confirm the analogue affinity of GLP-1 and the GLP-1 receptor’s specificity the invitro binding assay basically performed. This is a competitive binding assay that employs basically radiolabeled GLP-1 analogue. The binding affinity of this assay and the occupancy of the receptor GLP-1 analog are basically determined the helping the selecting the most potent type of candidate for the again evaluation.
In Vivo pharmacokinetic studies:
This research study is very crucial for understanding the distribution, absorption and different metabolism and ADME excretion for the GLP-1 analog of the living organism. There are different animal models like non-human primates or rodents are basically used to identify the behaviour of different analogs. This is the administration through different routes like oral, intravenous and the root of subcutaneous.
GLP-1Half life measurement
The analog of GLP-1 half-life is an important pharmacokinetic parameter that basically influences the frequency of dosing and the efficacy of treatment (Gilroy, et al. 2020). The half-life is basically determined through the measuring of the blood concentration rate over time after the administration process. The fluorescently and radioactive labels basically tagged the analogous that is used in the accurate amount of quantification.
GLP-1 Analog efficacy studies
This is the in-vivo efficacy study that is basically conducted for analyzing the ability of GLP-1 analog for improving the control level of glycemic and other relevant metabolic parameters also. The animal model for diabetes is basically streptozotocin-induced diabetic rate and this is basically used to assess the impact of analog on the “glucose level in the blood” and the “sensitivity of insulin” and for weight loss also.
Assessment of toxicity and safety
The evaluation of safety is an important aspect of the examination of GLP-1 peptides. The chronic and acute types of toxicity are basically conducted in the animal model that basically helps to investigate the potential type of adverse impact of this substance. The specific attention provides to the gastrointestinal system like GLP-1 analog that sometimes causes vomiting or nausea. As well as the immunological, cardiovascular and reproductive assessment would be performed.
Clinical trial
After the clinical studies, it has been demonstrated that the “GLP-1 analogs” basically progress to the clinical trial. These are conducted in the different phases that are associated with healthy volunteers for diabetic patients. Phase I basically focus on the tolerability and safety of this drug. Phase II basically assesses the efficacy of this drug and phase III evaluated the benefits of the drug and also describes the potential risk on a in large scale.
So that GLP-1 peptide testing is a critical test that is basically used for the treatment of diabetes in the targeting “GLP-1 pathway”. From the synthesis of the peptide to the efficacy of in Vivo and their safety evaluation. This is the comprehensive process that ensures the GLP-1 analogue that is basically optimized for clinical use (Górriz, et al. 2020). Through rigorous testing and the different evaluation process, these drugs have revolutionized and potential diabetes management. This is very essential to conducting the research and its clinical trial; that brings the novel GLP-1 analogue into the market which is finally improving the lives of millions of diabetic patients.
Compound 2
| Drug concentration | Control WT DNA | Mutant DNA | ||||
| 1.00E-03 | 8029 | 7964 | 8244 | 7922 | 8165 | 8027 |
| 1.00E-04 | 7949 | 7979 | 8132 | 7130 | 7209 | 7169 |
| 1.00E-05 | 6506 | 6267 | 6568 | 4217 | 4307 | 4205 |
| 1.00E-06 | 2345 | 2333 | 2367 | 601 | 628 | 639 |
| 1.00E-07 | 405 | 414 | 386 | 80 | 71 | 88 |
| 1.00E-08 | 90 | 76 | 68 | 90 | 82 | 74 |
| 1.00E-09 | 42 | 46 | 49 | 21 | 16 | 24 |
| B | 0 | 0 | 0 | 0 | 0 | 0 |
| drug concentration | CWT (Normalise) | Drug Concentration | Mutant DNA (Normalize) | |||
| 1.00E-03 | 8079 | 1.00E-03 | 8038 | |||
| 1.00E-04 | 8020 | 1.00E-04 | 7169.33 | |||
| 1.00E-05 | 6447 | 1.00E-05 | 4242 | |||
| 1.00E-06 | 2348.33 | 1.00E-06 | 622.66 | |||
| 1.00E-07 | 401.66 | 1.00E-07 | 79.66 | |||
| 1.00E-08 | 78 | 1.00E-08 | 82 | |||
| 1.00E-09 | 45.66 | 1.00E-09 | 20.33 | |||
GLP 1 Receptor
| Drug concentration | Control WT DNA | Mutant DNA | ||||
| 1.00E-05 | 7944 | 8114 | 8148 | 8239 | 8156 | 8257 |
| 1.00E-06 | 7111 | 7162 | 7239 | 7109 | 7133 | 7011 |
| 1.00E-07 | 7195 | 7213 | 7250 | 7061 | 7067 | 7178 |
| 1.00E-08 | 6604 | 6446 | 6678 | 6400 | 6550 | 6665 |
| 1.00E-09 | 4228 | 4025 | 4162 | 4159 | 4080 | 4245 |
| 1.00E-10 | 864 | 858 | 813 | 836 | 870 | 843 |
| 1.00E-11 | 69 | 60 | 68 | 73 | 75 | 68 |
| B | 0 | 0 | 0 | 0 | 0 | 0 |
| drug concentration | CWT (Normalise) | Drug Concentration | Mutant DNA (Normalize) | |||
| 1.00E-03 | 8068.66 | 1.00E-03 | 8217 | |||
| 1.00E-04 | 7170.66 | 1.00E-04 | 7012 | |||
| 1.00E-05 | 7219.33 | 1.00E-05 | 6654 | |||
| 1.00E-06 | 6576 | 1.00E-06 | 4399 | |||
| 1.00E-07 | 4138.33 | 1.00E-07 | 836 | |||
| 1.00E-08 | 845 | 1.00E-08 | 834 | |||
| 1.00E-09 | 65.66 | 1.00E-09 | 72 | |||
Ligand docking result
| scores | centers | ||||||
| 0.999078 | [148.3800048828125, 139.27999877929688, 120.51000213623047] | ||||||
| 0.987749 | [122.37999725341797, 133.27999877929688, 116.51000213623047] | ||||||
Table: ligand docking result
(Source: Source: self-created in https://playmolecule.com/deepsite/)
Result of GLP-1 peptide synthesis:
The synthesis of “glucagon-like peptide-1 (GLP-1)” is a complicated procedure that is passes through with numerous stages to form the final peptide. From the intestine, the GLP-1 hormone is secreted and this act as crucial role in the homeostasis of glucose. That helps to facilitate the secretion of insulin hormone and as well as it decreases the glucagon level after a full meal. Due to its therapeutic potential for controlling “type 2 diabetes synthetic GLP-1” has been subjected to considerable research.
From the “solid-state of peptide synthesis (SPSS)”, the GLP-1 synthesis begins. In this procedure, the chain of the peptide is formed with amino acids at a time on solid-type support. That follows a particular sequence that is dictated by the target GLP-1 sequence. Each amino acid protecting group are selected carefully to allow accurate coupling and it helps to prevent undesired side reaction. When the chain of peptides is assembled perfectly the protecting groups are removed from the peptide chain and it cleaved with the solid support. After that purification procedures like high-performance chromatography are employed to isolate the crude GLP-1 from the reaction mixture (Hölscher, 2022). The crude GLP-1 peptide is subjected further to the analytical process like mass spectrometry and high-pressure liquid chromatography to assess its purity to confirm its identity. After this procedure, the purified synthetic GLP-1 peptide is prepared for the different application like in vitro studies that helps to understand the in-vivo studies to identify the therapeutic potential to control diabetes. This is very important to emphasize the synthesis of GLP-1 like any other peptide required the stringent quality to maintain the measure that allows the final product and safe for its intended application. Chemical modifications may be introduced to increase the stability and pharmacological properties. The overall synthetic GLP-1 has proven a valuable tool in the scientific research that may hold as a therapeutic agent for diabetes and that is related to metabolic disease.
Result of GLP-1 receptor binding assays
In the lab test there occur the GLP-1 receptor binding assay this test is used to “assess the binding affinity of the glucagon-like peptide 1 (GLP-1)”. This hormone is “secret from the intestine and play an important role in the homeostasis of glucose”. This hormone helps to stimulate the insulin hormone and also inhibits the secretion of glucagon which is the crucial therapeutic management for controlling the diabetes. In the investigation of a particular type of quantity of radiolabeled GLP-1 is incubated in the sample that is containing GLP-1 receptors particularly that is emanated from the expression of the tissues of these receptors like pancreatic cells or the cell lines to overexpress the GLP-1 receptors. The non-labelled GLP-1 competes with radiolabeled GLP-1 for binding with the receptor sites (Muzurović, et al. 2022). By measuring the amount of radiolabeled GLP-1 bound to the receptors, the researchers can examine the affinity of the binding capacity of GLP-1 to its receptors and the potency of GLP-1 in displacing the radiolabeled ligand.
The outcome of the GLP-1 receptor binding assay gives the beneficial information about GLP-1 analog efficacy and that is connected to the drug interacting with the GLP-1 receptor. This helps to the clinical and researchers to understand the molecular interchange and pharmacokinetics of Therapy which is based on GLP-1. This information is crucial for designing and optimizing the treatment for type 2 diabetic patients and other metabolic disorders (Nauck, et al. 2021). Simultaneously the assay can seek to recognize the potential adverse impact and cross-reactivity with other receptors that ensure the efficacy and safety of GLP-1 targeted therapies in medical applications.
Finally, the GLP-1 receptor binding assay is used as a fundamental tool in the development of the drug for diabetes the aim of the research is to improving their controlling the diabetes management and its related conditions also.
Discussion
GLP-1 receptor works as an agonist in the class of medication that is used basically for treating diabetes mellitus. This is work as the stimulating of the GLP-1 receptor that can lead to enhance the secretion of insulin. This element helps to decrease the secretion of glucagon delaying gastric emptying and also increasing satiety (Muzurović, et al. 2022). These impacts contribute to the control of blood glucose and help to control the potential weight loss management. Over the year this element study has indicated that GLP-1 receptor antagonist has a beneficial impact on body weight and helps to measure the metabolic parameters of the body that basically used for treating obesity and metabolic disorders like prediabetes and diabetes. The efficacy and safety of this medication also vary. Further research will be needed to know the full potential of the drug.
According to Napoli, et al. (2021) in their research study, focused on the advantageous impact of glucagon-like peptide 1 receptor agonists that is the different aspects of the management of diabetes and this is associated to comorbidities. These are the class of medication that is basically used to control type 2 diabetes by mimicking the impact of the naturally occurring GLP-1 hormone, that regulate the level of blood glucose. Their research study investigated that the effect of GLP-1 RAs has an impact on the control of glucose also use the risk profile of cardiovascular disease and also use “fatty liver disease” in individuals who have “type 2 diabetes”. The outcome of this research study defines that GLP-1 RAs have a significant positive outcome on the control of glucose in the blood and it led to improving the body’s glycemic level which basically helps to manage diabetes (Napoli, et al. 2021). This medication was found a positive effect on cardiovascular risk factors this medication reduces blood pressure and also helps to improve the lipid profile in the body. This also potentially lowers the risk of complications of cardiovascular disease in diabetic patients. Their research study also focuses on the potential advantage of GLP-1 RAs that manage NAFLD. This is a well-known liver condition that is involved in resistance to insulin and obesity in type 2 diabetes patients. This medication is very helpful for the patient. So overall the Italian diabetes society also supported the GLP-1RAs that can the versatile and effective treatment of type 2 diabetes. These findings have an important implication for the clinical “management of diabetes” and this is associated with reducing complications, finally this lead to improving the condition of the patients.
According to Wright, et al. (2022), the aim of their research is to identify the efficacy of 2 classes of antidiabetic medications. In their research, they research SGLT2 inhibitors and GLP-12 receptors that are the initial “prevention of heart failure” and cardiovascular events in “type 2 diabetic patients”. This research explored the potential benefit of using the combination of using these medications and their outcome to improve diabetic conditions. This research study followed the randomized control trial that is include type 2 diabetes and cardiovascular disease. For this research, the participants are divided into 4 groups. One group of participants are receiving SGLT2 inhibitors and another group of participants receive GLP-1 receptors and third group of participants receive a combination of both medications and the fourth group of participants receive standard diabetic control care (Wright, et al. 2022). In this research study, the researchers closely monitored the participants in cardiovascular events like heart attacks, and strokes. They also assessed the other associated parameters like blood pressure, glycemic control and the renal function of the patients. The outcome of this research study has been demonstrating that both SGLT2 inhibitors and GLP-1 receptor antagonize are independently leading to a significant reduction of cardiovascular and heart failure occurrence that is compared to the standard diabetic care group. The combination of this therapy of both classes showed the greater advantages that help to the reduction of these events and focus on the potential synergistic impact also. This research study also provided strong evidence of the initial “prevention of heart failure” and cardiovascular events in “type 2 diabetic patients”. The usage of “GLP-1 receptor agonists” and SGLT2 inhibitors is a combination of therapy that could be a promising strategy to improve the long-term outcome and overall cardiovascular health of type 2 diabetic patients.
According to Ferrari, et al. (2022) in their research study, they demonstrate “GLP-1 Ras” that are generally used to “treat type 2 diabetes”. This basically works to stimulate the GLP-1 receptor which leads to an increase in the secretion of insulin which decreases the release of glucagon this helps to slow down gastric emptying and also helps to reduce appetite. These impact help to improve the control of blood glucose this has shown the effect in decreasing the cardiovascular risk factors. Past research has demonstrated that GLP-1 RAs did not generally improve the control of the glycemic rate but this also advantageous impact on cardiovascular results, which includes basically decreasing the risk of the adverse impact of cardiovascular events like heart attack, death due to cardiovascular disease and stroke (Ferrari, et al. 2022). The present research proceeds with the existing knowledge that potentially evaluates the “long-term cardiovascular impact of GLP-1 Ras” in patients that examining the different GLP-1 RA’s comparative efficacy and as well as the safety efficacy that has to a potential mechanism of cardiovascular protection in the glycemic control. The researchers also investigate the novel formulation or the different combination therapies to increase “the cardiovascular benefit of GLP-1 Ras”.
According to Onoviran, et al. (2019), the aim of their research study is to identify the effect of the glucagon-like peptide 1 receptor agonist in the older patient who is suffering from diabetes mellitus. GLP-1 RAs are the class that is commonly utilized to treat type 2 diabetes that has been shown the potential advantage of glycemic control and that specifically improve the comorbidities that are involved with “type 2 diabetes”. The research study approved the “randomized controlled trial” that is associated with 65 and older patients. That is associated with diabetes mellitus and cardiovascular disease and obesity. For this research, the researchers divided the participants into 2 groups. One group of people receive GLP-1 RAs and they are existing on diabetes therapy management and the other group of patients receive the without GLP-1 RAs (Onoviran, et al. 2019). This research study basically monitored the patients who are receiving glycemic control and the progression and management of the comorbidities. These patients also assessed the relevant health parameters like blood pressure, body weight, lipid profile etc. the result of this research showed that the group of people who are receiving GLP-1 RAs demonstrate significant improvement in the different comorbidities that are associated with diabetes Mellitus. These improvements include the better management of the risk of cardiovascular disease and help to reduce blood pressure and improve the lipid profile of the body. This GLP-1 RA group showed better glycemic control that is compared to the standard group. Based on the finding of the research the author summarized that GLP-1 RA can be a valuable treatment procedure that is basically used for diabetic mellitus patients. They help to control the blood sugar but it helps to give an advantageous effect on the comorbid conditions. This study focuses on the potential GLP-1 RA to enhance the overall health and well-being of older diabetic patients with multiple comorbidities.
According to Tanday, et al. (2021) in their research study they identified the potential advantages of adjunct therapies to improve the antidiabetic actions of “glucagon-like peptide-1 (GLP-1)”. This hormone occurs naturally and plays an “important role in glucose homeostasis”. This hormone helps to promote the secretion of insulin hormone and also suppresses the glucagon release. This therapeutic potential is restricted due to its short half-life and this is rapidly degraded in the body. The researchers investigate the feasibility of augmenting GLP-1’s impact by the different therapies that helps to improve the overall efficacy of controlling the diabetes. The finding of the resaerch uses different adjacent therapy to amplify the GLP-1’s antibiotic action. Through the combining of the GLP-1 analogue, the researchers observed an important improvement in glycemic control. The adjacent therapies help to prolong the half-life of GLP-1. That helps to prevent fast degradation and that enhancing bioavailability. The combination of different examinations demonstrates to increase glucose-lowering effect compared to GLP-1 receptor agonists. In their research, they also investigate the weight management of the patient and also helps to decrease the side effect that is involved with GLP-1-based treatments (Tanday, et al. 2021). This research identified that new adjunct therapies have the potential to revolutionize the treatment of the diabetes through the more sustainable and efficient glycemic control in diabetic patients. In their resaerch, they highlight the possibilities of the new adjunct therapies to amplify the antidiabetic actions. This offers to develop an improved treatment for diabetes that addresses some limitation factors also. Further research is also needed and many more “medical related trials are required” to translate and validate the findings of the practical therapeutic options of this drug for human use.
Conclusion
The safety assessment has indicated a favourable profile creating compound 2 attractive for further development. If it is proven successful in human trials this compound could be revolutionized the prevention of diabetes and significantly improve the quality of health and well-being. In conclusion, Compound 2 represents a battle against diabetes that holds the potential landscape of diabetes. Compound 2 may battel the way for a healthier future free from diabetes for countless individuals worldwide. This assignment has discussed different laboratory tests that are GLP-1 peptide synthesis, In Vivo pharmacokinetic studies, and In Vivo pharmacokinetic studies through this study it helps to know the binding affinity with the receptors of GLP-1. From the different literature, it has been known that this is a very effective drug used to control diabetes-like metabolic disorders.
Reference list
Journals
Batista, A.F., Bodart-Santos, V., De Felice, F.G. and Ferreira, S.T., 2019. Neuroprotective actions of glucagon-like peptide-1 (GLP-1) analogues in Alzheimer’s and Parkinson’s diseases. CNS drugs, 33(3), pp.209-223.
Bossart, M., Wagner, M., Elvert, R., Evers, A., Hübschle, T., Kloeckener, T., Lorenz, K., Moessinger, C., Eriksson, O., Velikyan, I. and Pierrou, S., 2022. Effects on weight loss and glycemic control with SAR441255, a potent unimolecular peptide GLP-1/GIP/GCG receptor triagonist. Cell metabolism, 34(1), pp.59-74.
Brown, E., Wilding, J.P., Barber, T.M., Alam, U. and Cuthbertson, D.J., 2019. Weight loss variability with SGLT2 inhibitors and GLP‐1 receptor agonists in type 2 diabetes mellitus and obesity: mechanistic possibilities. Obesity Reviews, 20(6), pp.816-828.
Chia, C.W. and Egan, J.M., 2020. Incretins in obesity and diabetes. Annals of the New York Academy of Sciences, 1461(1), pp.104-126.
Ferrari, F., Scheffel, R.S., Martins, V.M., Santos, R.D. and Stein, R., 2022. Glucagon-like peptide-1 receptor agonists in type 2 Diabetes mellitus and cardiovascular disease: the past, present, and future. American Journal of Cardiovascular Drugs, 22(4), pp.363-383.
Gilroy, C.A., Capozzi, M.E., Varanko, A.K., Tong, J., D’alessio, D.A., Campbell, J.E. and Chilkoti, A., 2020. Sustained release of a GLP-1 and FGF21 dual agonist from an injectable depot protects mice from obesity and hyperglycemia. Science advances, 6(35), p.eaaz9890.
Goldenberg, R.M., Cheng, A.Y., Fitzpatrick, T., Gilbert, J.D., Verma, S. and Hopyan, J.J., 2022. Benefits of GLP-1 (glucagon-like peptide 1) receptor agonists for stroke reduction in type 2 diabetes: a call to action for neurologists. Stroke, 53(5), pp.1813-1822.
Górriz, J.L., Soler, M.J., Navarro-González, J.F., García-Carro, C., Puchades, M.J., D’Marco, L., Martínez Castelao, A., Fernández-Fernández, B., Ortiz, A., Górriz-Zambrano, C. and Navarro-Pérez, J., 2020. GLP-1 receptor agonists and diabetic kidney disease: a call of attention to nephrologists. Journal of clinical medicine, 9(4), p.947.
Helmstädter, J., Keppeler, K., Küster, L., Münzel, T., Daiber, A. and Steven, S., 2022. Glucagon‐like peptide‐1 (GLP‐1) receptor agonists and their cardiovascular benefits—The role of the GLP‐1 receptor. British journal of pharmacology, 179(4), pp.659-676.
Hölscher, C., 2022. Protective properties of GLP‐1 and associated peptide hormones in neurodegenerative disorders. British journal of pharmacology, 179(4), pp.695-714.
Kabahizi, A., Wallace, B., Lieu, L., Chau, D., Dong, Y., Hwang, E.S. and Williams, K.W., 2022. Glucagon‐like peptide‐1 (GLP‐1) signalling in the brain: From neural circuits and metabolism to therapeutics. British Journal of Pharmacology, 179(4), pp.600-624.
Malik, F. and Li, Z., 2022. Non‐peptide agonists and positive allosteric modulators of glucagon‐like peptide‐1 receptors: Alternative approaches for treatment of type 2 diabetes. British Journal of Pharmacology, 179(4), pp.511-525.
Muzurović, E.M., Volčanšek, Š., Tomšić, K.Z., Janež, A., Mikhailidis, D.P., Rizzo, M. and Mantzoros, C.S., 2022. Glucagon-like peptide-1 receptor agonists and dual glucose-dependent insulinotropic polypeptide/glucagon-like peptide-1 receptor agonists in the treatment of obesity/metabolic syndrome, prediabetes/diabetes and non-alcoholic fatty liver disease—current evidence. Journal of Cardiovascular Pharmacology and Therapeutics, 27, p.10742484221146371.
Napoli, R., Avogaro, A., Formoso, G., Piro, S., Purrello, F., Targher, G. and Consoli, A., 2021. Beneficial effects of glucagon-like peptide 1 receptor agonists on glucose control, cardiovascular risk profile, and non-alcoholic fatty liver disease. An expert opinion of the Italian diabetes society. Nutrition, Metabolism and Cardiovascular Diseases, 31(12), pp.3257-3270.
Nauck, M.A., Quast, D.R., Wefers, J. and Pfeiffer, A.F., 2021. The evolving story of incretins (GIP and GLP‐1) in metabolic and cardiovascular disease: a pathophysiological update. Diabetes, Obesity and Metabolism, 23, pp.5-29.
Nauck, M.A., Wefers, J. and Meier, J.J., 2021. Treatment of type 2 diabetes: challenges, hopes, and anticipated successes. The Lancet Diabetes & Endocrinology, 9(8), pp.525-544.
Onoviran, O.F., Li, D., Toombs Smith, S. and Raji, M.A., 2019. Effects of glucagon-like peptide 1 receptor agonists on comorbidities in older patients with diabetes mellitus. Therapeutic advances in chronic disease, 10, p.2040622319862691.
Tanday, N., Flatt, P.R. and Irwin, N., 2021. Amplifying the antidiabetic actions of glucagon‐like peptide‐1: Potential benefits of new adjunct therapies. Diabetic Medicine, 38(12), p.e14699.
Tanday, N., Flatt, P.R. and Irwin, N., 2022. Metabolic responses and benefits of glucagon‐like peptide‐1 (GLP‐1) receptor ligands. British Journal of Pharmacology, 179(4), pp.526-541.
Thomas, M.K., Nikooienejad, A., Bray, R., Cui, X., Wilson, J., Duffin, K., Milicevic, Z., Haupt, A. and Robins, D.A., 2021. Dual GIP and GLP-1 receptor agonist tirzepatide improves beta-cell function and insulin sensitivity in type 2 diabetes. The Journal of Clinical Endocrinology & Metabolism, 106(2), pp.388-396.
Wright, A.K., Carr, M.J., Kontopantelis, E., Leelarathna, L., Thabit, H., Emsley, R., Buchan, I., Mamas, M.A., van Staa, T.P., Sattar, N. and Ashcroft, D.M., 2022. Primary prevention of cardiovascular and heart failure events with SGLT2 inhibitors, GLP-1 receptor agonists, and their combination in type 2 diabetes. Diabetes Care, 45(4), pp.909-918.
Yaribeygi, H., Sathyapalan, T. and Sahebkar, A., 2019. Molecular mechanisms by which GLP-1 RA and DPP-4i induce insulin sensitivity. Life sciences, 234, p.116776.
Zhao, P., Liang, Y.L., Belousoff, M.J., Deganutti, G., Fletcher, M.M., Willard, F.S., Bell, M.G., Christe, M.E., Sloop, K.W., Inoue, A. and Truong, T.T., 2020. Activation of the GLP-1 receptor by a non-peptidic agonist. Nature, 577(7790), pp.432-436.
Know more about UniqueSubmission’s other writing services:

