MBB7056M Healthcare Management Assignment Sample
Module code and Title: MBB7056M Healthcare Management Assignment Sample
Introduction
Pain indicates tissue damage which can be due to several medical problems. When the pain lasts for an extended period, it is referred to as chronic pain. The pain lasting more than three months is defined as chronic pain by the International Association for the Study of Pain. This type of pain occurs usually under any disease process or from the expected time following for an injury to heal (Hylands-White et al., 2017).
As a major source of suffering, chronic pain is accompanied by distress and is a leading source of human disability and suffering. However, the diseases associated with chronic pain are not always immediately life-threatening. Therefore, pain management should be regulated by patient-reported severity of its long-term conditions.
The International Association for the Study of Pain (IASP) has thus distinguished chronic pain into secondary and primary pain syndromes while integrating the existing pain diagnosis, providing accurate definitions with additional characteristic features of the respective diagnoses based on the WHO content model for ICD-11 (Treede et al., 2019).
The 2017 Global Burden of Disease Study estimated that the number of patients suffering from chronic pain is increasing, becoming the leading cause of disability throughout the world (Pain management techniques: 13 ways to manage chronic pain, 2022). Various treatments are also involved in pain management to improve their coping strategies. Thus chronic pain management is a holistic way aiming to improve the quality of life.
Literature review
Being a common public health problem, chronic pain has a detrimental impact on the patient’s quality of life and functions redefining itself as a distinct disease rather than a symptom of illness or injury. Chronic pain is associated with psychological challenges, involving symptoms of anxiety, depression and emotional distress, besides physical symptoms.
It also reduces the work productivity and unemployment issues impacting the socioeconomic condition of the patient. Its complex nature and multifaceted impact on the patients’ lives have made it necessary for chronic pain management to involve follow-ups from a wide range of health care providers.
Pain management should be devised to reduce pain while maximising the quality of life and improving functioning. Effective management of chronic pain is essential with its power to affect a large proportion of the general population which amounts to one in five adults, impacting the wider society considerably (Kress et al., 2015).
20% of the adult European population, mainly women and elders exhibit this serious health care problem (A Morrone et al., 2017). Multidisciplinary and comprehensive chronic pain management when applied appropriately with its specialised strategies and treatments has been found clinically effective. This pain management benefitted the patients by consistently improving their conditions.
Chronic pain management integrates various humanistic, clinical and economic factors (Provenzano et al., 2018). This pain management focuses on addressing the effects of pain for maximising the quality of life and functioning which is different from acute pain management addressing the cause of the pain. Rehabilitation is promoted rather than achieving a cure in chronic pain management (Mills et al., 2016).
This pain management technique involves physical therapy, acupuncture, yoga, medicinal cannabis or opioids. Various pharmacological, neuromodulation and behavioural strategies also aid pain management. Psychological interventions are also found effective for chronic pain management (Morley and Williams, 2015).
During the Covid-19 pandemic, chronic pain patients were uniquely challenged creating new barriers to receiving the treatment while increasing their stress to exacerbating chronic pain. Exacerbation symptoms were experienced by those patients due to personal and public health issues during the pandemic. The pandemic potentially increased the prevalence of chronic pain with the extension of stressors over many months. Long-term multidisciplinary management is also required for chronic patients even during the pandemic.
Anxiety, fear of abandonment and depression increased during the social isolation aggravated the pain conditions. Chronic pain management was affected worldwide with the shutting down of the pain services impacting the patients’ psychological health. The delivery of effective pain management thus became challenging (Puntillo et al., 2020). Although physical consultancies were reduced, biopsychosocial care was prioritised during that period.
The chronic patients, mostly elderly persons, with multiple comorbidities faced the potential risk of emotional and functional decline. This was mainly because of the increased burden on healthcare (Chan and Liu, 2020). Delays in the pain services thus promoted the long-term health disparities implicating rehabilitations within healthcare systems.
It is a serious challenge for the public healthcare system and authorities around the world for effective chronic pain management where around 28 million adults are affected by chronic pain in the UK (Hadi et al., 2017). Over 5 million people develop chronic pain in the UK every year, of whom only two-thirds recover (Macdonald et al., 2018). The increased prevalence of chronic pain, especially with disability and comorbidities, overlaps the risk of Covid-19.
According to UK Government research, chronic pain is prevalent with advancing age and those above 65 years of age are more exposed to the health issue (McGhie and Grady, 2016). Chronic pain is emerging as a significant issue in the UK pain management system which is poorly resourced and staffed for managing this issue. The healthcare organisations thus work constructively to improve chronic pain management in the UK.
The prescribed opioid use is found to be increasing in the UK for managing chronic pain. However, there are regional variations in the use of opioids in the UK. North of England accounts for 90% of the use of this drug (Alenezi et al., 2021). There is a lack of adequate addiction treatment and chronic pain is prevalent in greater numbers in the socio-economically deprived regions.
An emerging therapeutic option for primary chronic pain is implementing cannabis-based medical products. This approach involves modulating the peripheral and central pain processes with the help of an endocannabinoid system. This treatment has resulted in improving pain-specific outcomes in the UK (Kawka et al., 2021).
40% of the UK adult population affected by chronic pain represents a significant global burden at socio-economic and individual levels (Fallon et al., 2021). These chronic pain populations can be found to be disproportionately affected by the pandemic health restrictions with reduced access to healthcare increasing the risk of disease severity from being affected by Covid-19. Under such situations, self-management strategies adhering to the prescribed medication and regimes played a significant role in chronic pain management.
The strategy helped in psychological coping with pain intervention while identifying the pain by consulting with a medical practitioner. However, this strategy is also impacted by socio-economic status, which creates a lack of resources during hard times. The pandemic has also brought burden and risk to these affected populations with their disease management severely affecting their well-being mitigating possible risks in future waves of the pandemic. However, post the lockdown, no such improvements were noticed among the chronic pain population (Zambelli et al., 2022).
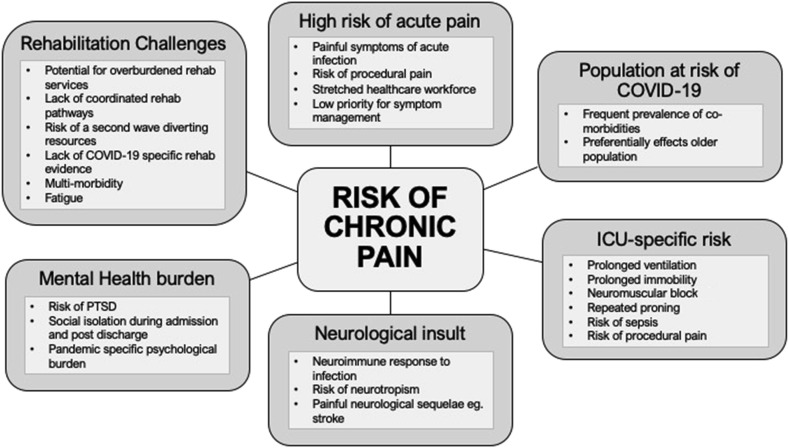 Figure 1: (Source: Kemp et al., 2020)
Figure 1: (Source: Kemp et al., 2020)
Chronic pain conditions often create increased risks for individuals of social isolation with reduced functioning roles in society. With the presentation of complex physical and mental health comorbidities, the multiple health system touchpoints and the multifaceted nature of pain have complicated chronic pain management. This strategic management also focuses on opioid reduction. However, with the lack of resources, the chronic pain management approaches fail to get recognised.
The lack of time and resources prevents clinicians to manage chronic pain holistically and fosters variations in care (Cate Polacek et al., 2020). Each patient with chronic pain should be knowledgeable and access the pain management interventions regardless of their geographical location. Self-management interventions also stimulate chronic pain management, promoting patients to actively participate in treatments rather than depending on pharmacologic interventions which are mostly opioid based (Eaton et al., 2018).
Conclusion
The increased stressors during the pandemic also increased chronic pain patients with long-term consequences. The pandemic created a huge shift in the patient’s healthcare and social activities. Chronic pain patients entering the pandemic with fewer social resources under social isolation are also filled with loneliness. The life stressors brought by the pandemic have also increased the need for pain services. However, their potential impact on health can be mitigated by recognising new and pre-existing chronic pains and employing prompt treatment.
It was also worsened by the psychological stresses due to the pandemic. Scientific attention can prevent the increase in the severe impact of chronic pain to develop new ways to provide pain management among chronic patients. Thus, it is inevitable to review the pain management practices while re-allocating healthcare resources, infection control measures, analgesic use, community collaborations and pain interventions even during critical times like the Covid-19 pandemic. Biopsychosocial and interdisciplinary approaches toward chronic pain management are however found to be the most effective practice during the pandemic.
Some commissioning services in the UK chronic pain management services can be incorporated into their plan to handle the chronic issues:
- To prevent and reduce chronic pain disabilities integration of public health services and early interventions at community levels can be encouraged
- To ensure the availability of self-management principles, early biopsychosocial assessments can be developed within the community settings to serve those with chronic pain conditions.
- To utilise pathway mapping, tested data collection tools, and service development tools for modernising the service deliveries through trained caregivers
- To develop multidisciplinary teams and care pathways to support those chronic patients within local communities to remove their fear of isolation.
References
Cate Polacek, M.L.I.S., Christopher, R., Mann, M. and Udall, M., 2020. Healthcare professionals’ perceptions of challenges to chronic pain management. The American journal of managed care, 26(4), pp.e135-e139.
Chan, D.X. and Liu, C.W., 2020. Clinical challenges and considerations in management of chronic pain patients during a COVID-19 pandemic. Pain.
Eaton, L.H., Langford, D.J., Meins, A.R., Rue, T., Tauben, D.J. and Doorenbos, A.Z., 2018. Use of self-management interventions for chronic pain management: a comparison between rural and nonrural residents. Pain Management Nursing, 19(1), pp.8-13.
Fallon, N., Brown, C., Twiddy, H., Brian, E., Frank, B., Nurmikko, T. and Stancak, A., 2021. Adverse effects of COVID-19-related lockdown on pain, physical activity and psychological well-being in people with chronic pain. British journal of pain, 15(3), pp.357-368.
Hadi, M.A., Alldred, D.P., Briggs, M., Marczewski, K. and Closs, S.J., 2017. ‘Treated as a number, not treated as a person’: a qualitative exploration of the perceived barriers to effective pain management of patients with chronic pain. BMJ open, 7(6), p.e016454.
Hylands-White, N., Duarte, R.V. and Raphael, J.H., 2017. An overview of treatment approaches for chronic pain management. Rheumatology international, 37(1), pp.29-42.
Kawka, M., Erridge, S., Holvey, C., Coomber, R., Usmani, A., Sajad, M., Platt, M.W., Rucker, J.J. and Sodergren, M.H., 2021. Clinical Outcome Data of First Cohort of Chronic Pain Patients Treated With Cannabis‐Based Sublingual Oils in the United Kingdom: Analysis From the UK Medical Cannabis Registry. The Journal of Clinical Pharmacology, 61(12), pp.1545-1554.
Kemp, H.I., Corner, E. and Colvin, L.A., 2020. Chronic pain after COVID-19: implications for rehabilitation. British journal of anaesthesia, 125(4), pp.436-440.
Kress, H.G., Aldington, D., Alon, E., Coaccioli, S., Collett, B., Coluzzi, F., Huygen, F., Jaksch, W., Kalso, E., Kocot-Kępska, M. and Mangas, A.C., 2015. A holistic approach to chronic pain management that involves all stakeholders: change is needed. Current medical research and opinion, 31(9), pp.1743-1754.
Macdonald, M., Vaucher, P. and Esteves, J.E., 2018. The beliefs and attitudes of UK registered osteopaths towards chronic pain and the management of chronic pain sufferers-a cross-sectional questionnaire-based survey. International Journal of Osteopathic Medicine, 30, pp.3-11.
McGhie, J. and Grady, K., 2016. Where now for UK chronic pain management services?. BJA: British Journal of Anaesthesia, 116(2), pp.159-162.
Medicalnewstoday.com. 2022. Pain management techniques: 13 ways to manage chronic pain. [online] Available at: <https://www.medicalnewstoday.com/articles/pain-management-techniques#drug-therapy> [Accessed 6 August 2022].
Mills, S., Torrance, N. and Smith, B.H., 2016. Identification and management of chronic pain in primary care: a review. Current psychiatry reports, 18(2), pp.1-9.
Morley, S. and Williams, A., 2015. New developments in the psychological management of chronic pain. The Canadian Journal of Psychiatry, 60(4), pp.168-175.
Provenzano, D.A., Kamal, K.M. and Giannetti, V., 2018. Evaluation of primary care physician chronic pain management practice patterns. Pain Physician, 21(6), pp.E593-e602.
Puntillo, F., Giglio, M., Brienza, N., Viswanath, O., Urits, I., Kaye, A.D., Pergolizzi, J., Paladini, A. and Varrassi, G., 2020. Impact of COVID-19 pandemic on chronic pain management: Looking for the best way to deliver care. Best Practice & Research Clinical Anaesthesiology, 34(3), pp.529-537.
Treede, R.D., Rief, W., Barke, A., Aziz, Q., Bennett, M.I., Benoliel, R., Cohen, M., Evers, S., Finnerup, N.B., First, M.B. and Giamberardino, M.A., 2019. Chronic pain as a symptom or a disease: the IASP Classification of Chronic Pain for the International Classification of Diseases (ICD-11). pain, 160(1), pp.19-27.
Zambelli, Z., Fidalgo, A.R., Halstead, E.J. and Dimitriou, D., 2022. Acute impact of a national lockdown during the COVID-19 pandemic on wellbeing outcomes among individuals with chronic pain. Journal of health psychology, 27(5), pp.1099-1110.
Know more about UniqueSubmission’s other writing services:

