MOD007207 Summative Assessment Sample
Essential Knowledge and Skills for Person-Centred Care
1.Introduction
The chosen patient group is the discussion about obesity in adults’ groups within the community of the UK. The gender and age group for the identification will be from 19-70 years targeting both the male and female gender of the UK. Obesity can have a number of vulnerabilities among the patient’s group due to the stereotypical mindset of society (Wharton et. al. 2020). And in this essay, the information of the patient group with obesity targeting the adults in the UK will be shown as the background of the topic. The second part will show the stereotyping group of behaviour among the society towards the patient’s groups explaining the reason behind the behaviour. The impact of stereotyping among the patient’s group, the health issues, and access to health care with the societal pressure. Explaining in the next part about the strategies to plan as nursing for empowering the patients and society for effective improvement in vulnerabilities. While also reflecting on the values and beliefs an individual learned from this analysis.
2. Background Information
The commonality of the patient’s group is obesity in adults. This illness has tripled worldwide since 1975 and in 2016 more than 1.6 billion adults were overweight across many countries. And overweight is the cause for many people being killed than the underweight disease (Wadden et. al. 2020). The fundamental cause for the commonality of the disease among adults is due to lifestyle and food consumption imbalance that increases the high energy foods consumption consisting of fats and sugar.
2.1 Statistics
Obesity is defined as an abnormal increase in the amount of fat within the human body that may increase complications among human bodies. The main cause for obesity is the imbalance in consuming calories and the common impact of obesity is Cardiovascular-disease leading to a heart attack (Inoue et. al. 2018). Musculoskeletal diseases of joints disability, cancers in breast, ovarian, kidney, gallbladder.
The adult becomes obese due to eating habits, medication consumption, inactivity, genetics, and mostly it causes diseases that are fatal. Diabetics, heart diseases, cancer, joint disability are some common diseases. The UK population majority is suffering from obesity with almost 60% in 2018. Overall, in the UK 67% of men and 60% of women were suffering from obesity (Harris et. al. 2018). The proportion of adults who were overweight was highest among men between 55 and 64 is 82% and women aged between 65 and 74 (70%). The ratio of adults was highest among men between 45 to 54 (36%) and women are 37% between 55 to 64 years (Brayner et. al. 2021). The signs of obesity are high blood pressure, high cholesterol levels, joint pains, and breathing problems.
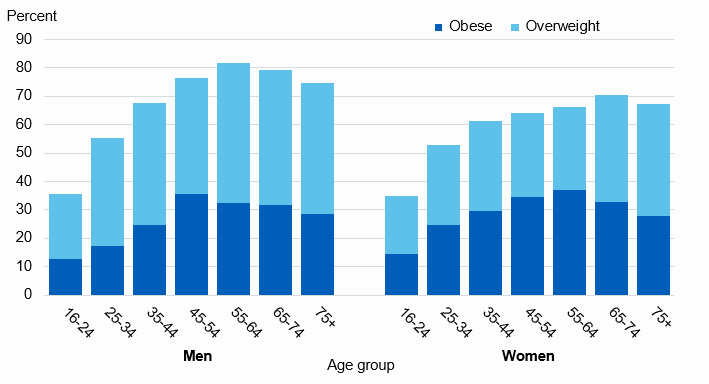
Figure 1 Age group
(Sources: Age group, 2020)
3. Stereotyping of the chosen group
A stereotyping is the belief of society about a particular group of people and an expectation that people have about a particular group and varies with groups personality, preferences, and ability in social groups. It is a process of overgeneralising, inappropriate, and resisting new information by society towards particular groups (Cooper et. al. 2018). The common stereotyping among UK society regarding the adult patient suffering from obesity is very prejudiced and rejected from various public affairs, choosing normal people over obese. People suffering from are seen by the group of society as weak, lazy, and sick that also reduces their chances to get jobs in the UK. The people suffering from obesity in universities as students face more weight bias and very little group favouritism due to their inactive physical well-being. They are tease and humiliated among friends’ group with the belief of making fun of overeaters. They are believed to be lazy and hazardous, boring, inactive on the contrary thin are supported to be attractive, healthy, active, and dedicated to life and work.
The stereotypical belief among the society in the UK is due to the modern theory of people considering thin and extra lean body as the definition of attractiveness, health-conscious, fit people that works hard (Konttinen, 2020). Society forces and disapprove of people suffering from obesity while walking down the streets. The peer’s belief, beauty products, athletes’ charismatic personalities have been some of the reasons for pressuring the patients suffering from obesity to negatively impact their life with various unethical comments, disapprovals among society. African Caribbean is part of obesity and minority UK ethnic groups with hypertension and genetics obesity that increase the racism among the society increasing the social disapproval (38 to 32% among women) (Noonan, 2021).
4. Impact of stereotyping
The impact of stereotyping among the patients suffering from obesity has increased the stress and insecurity among individuals that have to deteriorate the mental health of the patients. Among adults, the college and working group of people face this stereotype more due to peers’ pressure, family, and superiors among the obese patients to lose weight (Krzysztoszek et. al. 2019). Discrimination towards people suffering from obesity causes numerous consequences in their psychological and physical health. People suffering from obesity are blamed for their weight and provided various health activities to influence society to choose healthy eating behaviour. The constant societal discrimination among society increases their level of insecurity and mental stress. The stigma of weight discriminating people suffering from obesity for health awareness has threatened obese health generating health disparities causing a threat to the safety of the patients suffering from obesity.
The negative attitude of people towards people suffering from obesity in the UK has increased numerous harmful weight-based stereotypes that have affected their mental health (Kim et. al. 2017). The stereotype belief of people with obesity are lazy, lack self-discipline, have few will power, and are unintelligent, are very unsuccessful with non-compliant to lose weight due to negligence. The multiple domains of living in the workplace, health care centres, educational institutions, mass media with the stereotypical belief have increased the discrimination (Godziuk et. al. 2019). Enhancing the biasness causes insecurity for the patients suffering from people not considering getting treatment even in the health care centre. The discrimination among health care centre has increased the insecurity and fear of blame that influence patients suffering from people to minimise the treatments in health care centre regarding the obese disease. The social weight stigma has been a constant bias that has been frequently reported by teachers, physicians, medical students, psychologists, peers, friends, family. It is the reason for increasing the fear to approach health care centre for treatments. Avoiding to approach various physical activities in public out of fear and insecurity that potentially make their own life questionable in doing the things they prefer.
Throughout decades the people suffering from obesity are blamed in public for their careless eating habits letting them increase their weight which has allowed for stigma socially for humiliating them. The cause for mental disease, heart attacks, increases due to constant pressure from society. The depression and anxiety for non-acceptance of people suffering from obesity among peers have increased. In health care people suffering from obesity are mostly been targeted as lazy, lacking self-control to eat, and careless (Halliday et. al. 2020). Instead of treating patients, mostly healthcare is facilitating to aware the public for avoiding these problems with healthy eating habits. This type of social stigma is judging the patients of obese as more unhygienic which rise the bias and insecurity among the obese population to not opt for health care treatments. As result, almost 79% of people eat up more to release stress due to weight discrimination (Pimpin et. al. 2018). This eating disorder is the cause of more fatal diseases among people suffering from obesity with stereotypical bias among society in the UK.
Emotional and psychological problems are the result of discrimination among patients suffering from obesity in the UK. Society provides negative comments that impact the willpower of obese patients to confidently walk and believe in their skills. Lower self-esteem, anxiety, depression, cases of suicide are the major causes of obesity that have been a serious issue among society. The non-acceptance of society and judgments cause patients suffering obesity to have more mental health issues (Mun et. al. 2018). Individuals for society judgments are more likely to have 3-4 times higher depression than non-obese people. Another issue is due to low self-esteem for stereotypical judgments, people suffering from obesity are most likely to cope with the habit of having an eating disorder and isolating themselves from socialising due to pressure from the public. Almost 53% of the women receive discriminating comments in health care due to obesity (Burton et. al. 2021). 52% of women do not try to seek preventive measures in health care centre due to the discrimination and inappropriate comments that enhance the chance for fatal diseases among patients suffering from obesity (Zhu et. al. 2020).
Therefore, overcoming the discrimination among patients suffering from obesity requires strategies to empower them with the various implementation of policies for minimising the disease.
5. Strategies to promote inclusivity
The UK policy in 2020 has been about a health awareness campaign towards reducing obesity among people launched during the covid-19 pandemic. The better half campaign is a policy that the UK health department targeted to reduce obesity in the UK population (Perreault and Apovian, 2019). This plan is meant to provide guidance in losing weight with healthy dietary eating options considering a more active lifestyle plan for patients suffering from obesity to stay motivated towards losing weight. The main aim of the policy was to develop a positive health campaign to aware of the healthy eating lifestyle, tackle obesity, to overall lose weight with positive words rather than discriminating the patients suffering from obesity with negative words. The policy emphasised the NHS burden for treating the individuals with suggestions for not blaming patients suffering from obesity for their conditions. And suggested plan for NHS to treat the patients with care and live healthier weight without blame (Celis-Morales et. al. 2017).
The policy paper sets out the process of improving health; advertising less regarding unhealthy foods, improving the food labelling in shops, cafes, restaurants for the clear suggestion of calories to motivate patients suffering from obesity to lose weight. The awareness of stigma weight is not provided that is encouraging the society to accept the patients suffering from obesity to support lose weight without blaming or discriminating them as lazy, careless peoples (Perreault, 2018). So as a nurse the patients suffering from obesity with the above better health campaign support can aware of the healthy living lifestyles that will enhance their confidence in the health care centre. And lose unwanted weight for a healthy living lifestyle. The suggestion to consider the better health campaign by nurses to obese patients will encourage the patients as the guidelines show a positive image of the people suffering from obesity to lose weight. This policy will empower the patients of obese as this policy focus on eliminating the weight stigma with positive words to motivate patients suffering from obesity.
Guidelines provided by the better health campaign that nurses can use to empower the patients suffering from obesity are the buying of the grocery. The government with the new legislation is trying to provide restrictions on high-fat salt and sugar products by eliminating the buy one gets one free sales promotion in grocery shopping (Peralta et. al. 2018). The nurses with good awareness campaigns in health care can aware people suffering from obesity about the HFSS products. And aware about the business strategies that will only increase the level of sugar and fats in the body. And to ask each obese patient with the help of new obese health guidelines to check the labelling of each food product before buying for understanding the existence of calories to stop eating unhealthy foods for minimising the obese diseases in the UK (Anderson et. al. 2017).
On the other hand, individuals, or society can support patients suffering from with proper support towards the policies provided to people suffering from obesity by the UK government. Society must encourage patients suffering from obesity with various positive words for losing weight without discrimination (Biddle et. al. 2017). Society must support healthy eating campaigns organised by the UK government to support patients with obesity. The agricultural fresh foods, veggies, challenges in social media to promote eat healthy by individuals can encourage obese patients to stay healthy without stigma weight discrimination. Food active is a program for people to eat healthy foods for minimising disease risk. These programs must be encouraged by society to encourage patients with obesity for living a normal life without discrimination. Society instead of judging and blaming with negative stereotypical words. Rather should use goods motivational words to encourage patients for losing weight without making them anxious and self-alert about their weight negatively.
Another way is to volunteer to participate in physical activities training programs to help the patients suffering from obesity in public fitness campaigns supporting patients suffering from obesity without judging them. The depressed, anxious, anti-social patients suffering from obesity are increasing in the UK due to society prejudice (Dietz and Santos-Burgoa, 2020). And with effective support towards volunteering and motivating them will help to reduce depression, anxiety. And bring back the confidence to approach public health care centre and campaign for losing weight with a positive mindset without hesitation and fear of blame.
6. Reflection on self-awareness and resilience
The stereotypical belief of society has made me very conscious about the changes required to change the mindset of society towards patients suffering from obesity. The adult group of people who are obese is discriminated against and humiliated blaming them for the reason of the disease. They are judged for being lazy, untalented, careless people who lack skills for good employability (Roy and Uekusa, 2020). This kind of mindset of society has made me believe that people need to change and racism have been a serious cause for the increase in obesity among peoples. The patients are not approaching the help care centre for the humiliation and weight stigma for promoting the weight loss importance that is directly blaming the people suffering from obesity for the cause of the obesity disease. I felt very humiliated during the analysis as I too had the same mindset about people suffering from obesity and my behaviour towards the patients suffering from obesity was similar to the other stereotypical society mindset.
I am able to be very honest about the views of others as they are racist and judgemental towards the patients. They have been the reason for the patient’s low confidence and anti-social cause that have increased the rate of diseases among people suffering from obesity, depression, and suicidal rate. My opinion towards blaming people suffering from obesity for the cause of obesity among them has been a challenged opinion in learning. The learning has challenged me to change the opinion of blaming people suffering from obesity, stereotypical mindset as this has been the cause for their obesity, diseases, and anti-social distancing that have increased the rate of obesity.
Yes, after the whole analysis, the identification of the impact of stereotypical mindset and strategies to promote the policy for empowering patients suffering from obesity have changed my opinion. Now I feel I will like to change my mindset towards patients suffering from obesity. Encourage society to support obesity by volunteering in health programs to boost their willpower for losing weight and valuing their existence in society.
I have learned from the policy of better health campaign launched as the motive to boost obesity people to eat healthy by UK government. I have been learning to cope with the stereotypical action by considering to be aware of the obesity causes and reasons which will help to avoid blaming others (Crane et. al. 2020). And also, the aim of influencing the stereotypical mindset will be minimised by joining more awareness programs for supporting patients suffering from obesity. The connection towards the patients suffering from obesity and positive support will help to cope up with the stereotypical actions towards me. I will always know the cause of obese and I will support obese with guidelines to minimise the obese in society without any impact on me for judging obese patients.
I need to increase my emotion-focused to cope with the problems that society creates regarding the obese and with emotion-focused, I can connect with people suffering from obesity increasing my resilience for avoiding the stereotypical behaviours of society. The help of policy understanding and the impact of social prejudice upon people has increased my resilience to stay focused. And never judge others’ ability due to a society belief in humiliating others.
7. Conclusion
The first point of the essay showed the obesity and the reason for obesity that is impacting the health of patients suffering from obesity. The obesity in adult target groups and the reason for the obesity has improved the knowledge about the UK population impacted by obesity. The statistics have provided the exact number of age groups with gender affected by obesity. The UK group of people have been highly affected by obesity due to food habits and also due to the stereotypical behaviour of the society among patients suffering from obesity. The health care centre resistance, social isolation, depression were some mental health issues faced by patients suffering from obesity due to society’s stereotypical actions. The only way to minimise the patient suffering from obesity’s insecurity is the support from society and from the health care centre nurses empowering with UK health policy guidance to minimise the discrimination. The last self-reflection has shown the awareness I have gained from the analysis determining ways to avoid the stereotypical actions of society.
References
Anderson, S.E., Sacker, A., Whitaker, R.C. and Kelly, Y., (2017). Self-regulation and household routines at age three and obesity at age eleven: longitudinal analysis of the UK Millennium Cohort Study. International Journal of Obesity, 41(10), pp.1459-1466.
Biddle, S.J., Garcia, E.B., Pedisic, Z., Bennie, J., Vergeer, I. and Wiesner, G., (2017). Screen time, other sedentary behaviours, and obesity risk in adults: a review of reviews. Current obesity reports, 6(2), pp.134-147.
Brayner, B., Kaur, G., Keske, M.A., Perez-Cornago, A., Piernas, C. and Livingstone, K.M., (2021). Dietary patterns characterized by fat type in association with obesity and type 2 diabetes: a longitudinal study of UK Biobank participants. The Journal of Nutrition, 151(11), pp.3570-3578.
Burton, Z.A., Lewis, R., Bennett, T., McLernon, D.J., Network, P.A.T.R., Engelhardt, T., Brooks, P.B. and Edwards, M.R., (2021). Prevalence of PErioperAtive CHildhood obesitY in children undergoing general anaesthesia in the UK: a prospective, multicentre, observational cohort study. British journal of anaesthesia.
Celis-Morales, C.A., Lyall, D.M., Gray, S.R., Steell, L., Anderson, J., Iliodromiti, S., Welsh, P., Guo, Y., Petermann, F., Mackay, D.F. and Bailey, M.E., (2017). Dietary fat and total energy intake modifies the association of genetic profile risk score on obesity: evidence from 48 170 UK Biobank participants. International journal of obesity, 41(12), pp.1761-1768.
Cooper, C.B., Neufeld, E.V., Dolezal, B.A. and Martin, J.L., (2018). Sleep deprivation and obesity in adults: a brief narrative review. BMJ open sport & exercise medicine, 4(1), p.e000392.
Crane, M.F., Kho, M., Kangas, M., Griffin, B., Karin, E., Earl, J.K. and Harris, C.B., (2020). Strengthening resilience in over 50’s: A nested clustered-randomized controlled trial of adaptive systematic self-reflection. Anxiety, Stress, & Coping, 33(6), pp.623-641.
Dietz, W. and Santos-Burgoa, C., (2020). Obesity and its implications for COVID-19 mortality. Obesity (Silver Spring), 28(6), p.1005.
Godziuk, K., Prado, C.M., Woodhouse, L.J. and Forhan, M., (2019). Prevalence of sarcopenic obesity in adults with end-stage knee osteoarthritis. Osteoarthritis and cartilage, 27(12), pp.1735-1745.
Halliday, T.M., Rynders, C.A., Thomas, E., Bergouignan, A., Pan, Z., Kealey, E.H., Cornier, M.A. and Bessesen, D.H., (2020). Appetite‐related responses to overfeeding and longitudinal weight change in obesity‐prone and obesity‐resistant adults. Obesity, 28(2), pp.259-267.
Harris, L., Hamilton, S., Azevedo, L.B., Olajide, J., De Brún, C., Waller, G., Whittaker, V., Sharp, T., Lean, M., Hankey, C. and Ells, L., (2018). Intermittent fasting interventions for treatment of overweight and obesity in adults: a systematic review and meta-analysis. JBI Evidence Synthesis, 16(2), pp.507-547.
Inoue, Y., Qin, B., Poti, J., Sokol, R. and Gordon-Larsen, P., (2018). Epidemiology of obesity in adults: latest trends. Current obesity reports, 7(4), pp.276-288.
Kim, Y., Wijndaele, K., Lee, D.C., Sharp, S.J., Wareham, N. and Brage, S., (2017). Independent and joint associations of grip strength and adiposity with all-cause and cardiovascular disease mortality in 403,199 adults: the UK Biobank study. The American journal of clinical nutrition, 106(3), pp.773-782.
Krzysztoszek, J., Laudanska-Krzeminska, I. and Bronikowski, M., (2019). Assessment of epidemiological obesity among adults in EU countries. Annals of Agricultural and Environmental Medicine, 26(2).
Mun, J., Kim, Y., Farnsworth, J.L., Suh, S. and Kang, M., (2018). Association between objectively measured sedentary behavior and a criterion measure of obesity among adults. American Journal of Human Biology, 30(2), p.e23080.
Noonan, R.J., (2021). Family income matters! Tracking of habitual car use for school journeys and associations with overweight/obesity in UK youth. Journal of Transport & Health, 20, p.100979.
Peralta, M., Ramos, M., Lipert, A., Martins, J. and Marques, A., (2018). Prevalence and trends of overweight and obesity in older adults from 10 European countries from 2005 to 2013. Scandinavian journal of public health, 46(5), pp.522-529.
Perreault, L. and Apovian, C., (2019). Obesity in adults: Overview of management. UpTo-Date. Apr.
Perreault, L., (2018). Obesity in adults: drug therapy. Waltham: UpToDate.
Pimpin, L., Jebb, S.A., Johnson, L., Llewellyn, C. and Ambrosini, G.L., (2018). Sources and pattern of protein intake and risk of overweight or obesity in young UK twins. British Journal of Nutrition, 120(7), pp.820-829.
Roy, R. and Uekusa, S., (2020). Collaborative autoethnography:“self-reflection” as a timely alternative research approach during the global pandemic. Qualitative Research Journal.
Wadden, T.A., Tronieri, J.S. and Butryn, M.L., (2020). Lifestyle modification approaches for the treatment of obesity in adults. American Psychologist, 75(2), p.235.
Wharton, S., Lau, D.C., Vallis, M., Sharma, A.M., Biertho, L., Campbell-Scherer, D., Adamo, K., Alberga, A., Bell, R., Boulé, N. and Boyling, E., (2020). Obesity in adults: a clinical practice guideline. Cmaj, 192(31), pp.E875-E891.
Zhu, Z., Guo, Y., Shi, H., Liu, C.L., Panganiban, R.A., Chung, W., O’Connor, L.J., Himes, B.E., Gazal, S., Hasegawa, K. and Camargo Jr, C.A., (2020). Shared genetic and experimental links between obesity-related traits and asthma subtypes in UK Biobank. Journal of Allergy and Clinical Immunology, 145(2), pp.537-549.
Age group, (2020). [Online]. [Accessed through]:<https://digital.nhs.uk/data-and-information/publications/statistical/statistics-on-obesity-physical-activity-and-diet/england-2020/part-3-adult-obesity-copy>
………………………………………………………………………………………………………………………..
Know more about Unique Submission’s other writing services:

