Assignment Sample on BME802 Catheter Ablation for Atrial Fibrillation: Techniques and Existing Devices
Introduction
According to Zei et al., (2020), Atrial fibrillation of catheter ablation is an irregular heart rhythm that was measured by the rapid and abnormal beating of the atrial chamber. It is initiated at the beginning of a short period of abnormal beating and over time it becomes longer and conscious. For this patient atrial fibrillation catheter ablation is very significant for therapeutic intervention. It is understood that catheter ablation is more effective than antiarrhythmic drug therapy. It facilitates the maintenance of the middle-aged patient with paroxysmal AF in sinus rhythm. On the other hand, it is not well known the role of catheter ablation to other patients. The effect of catheter ablation is unknown to other patient groups that particularly for long-standing persistent AF, heart failure, and elderly people.
Over the several decades, catheter ablation of martial fibrillation has evolved and it is under the largely experimental procedure and it established therapeutic options for the certain disease (Pothineni et al., 2020). At present time the majority of the catheter ablation technique is dependent on the techniques that target the pulmonary vein. It controls the electrical isolation and maintains sinus rhythm. The optimal strategy that has been taken for the treatment of atrial fibrillation, the treatment is continuously evolving which causes challenges for clinicians that initiate and maintain martial fibrillation. The results from the composite interaction between arrhythmia triggers and altered the substrate of atrial and change in the activity of the autonomic nervous system. When a patient undergoes catheter ablation, the set of optimal ablations rely on the primary distribution of the factors and the clinical type of atrial fibrillation.The pathophysiology of martial fibrillation is involved with the interaction among the interaction triggers that have been framed in the form of the quick-firing of ectopic loci that is present inside the pulmonary veins and the substrate of atrial tissues which is capable to maintain the arrhythmia.
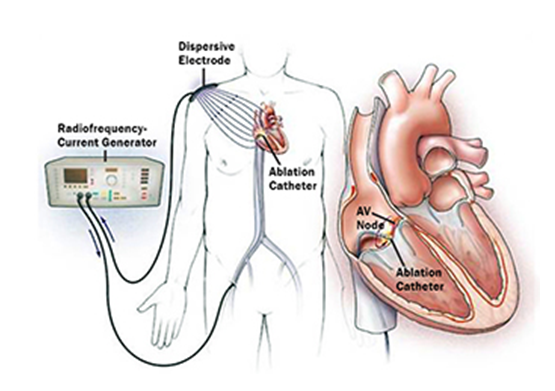
Figure 1: cardiac ablation
Source: (Zei et al., 2020)
General cardiac catheterization and ablation principles
The catheterization of ablation principle, is the method doctors administer a very small catheter which looks like a hollow tube, that is inserted into the blood vessel in the groin, arm, or in neck. The doctor inserted the thread into the blood vessels inside the aorta region of the heart (Ahn et al., 2021). After the catheter is pointed at the expected region that several diagnostic tests could be done. Moreover, doctors place a tip of the catheter into the different parts of the heart. It facilitates measuring the pressure inside the heart chambers. Also, it checked blood samples in order to measure the level of oxygen
In order to check blood flow inside the heart, doctors guide the catheter arteries and shoot up the dye. The coronary artery is a vessel that carries designated blood to the heart muscles. This is also regarded as coronary angiography (Cha et al., 2020). During this procedure, several aspects have been done after the administration of cardiac cathitar.
Angioplasty: in this procedure, the doctor inserted a small balloon at the upper tip of the catheter. This developed blood flow by pressing any plaque against the artery wall that improves the blood flow at the artery.
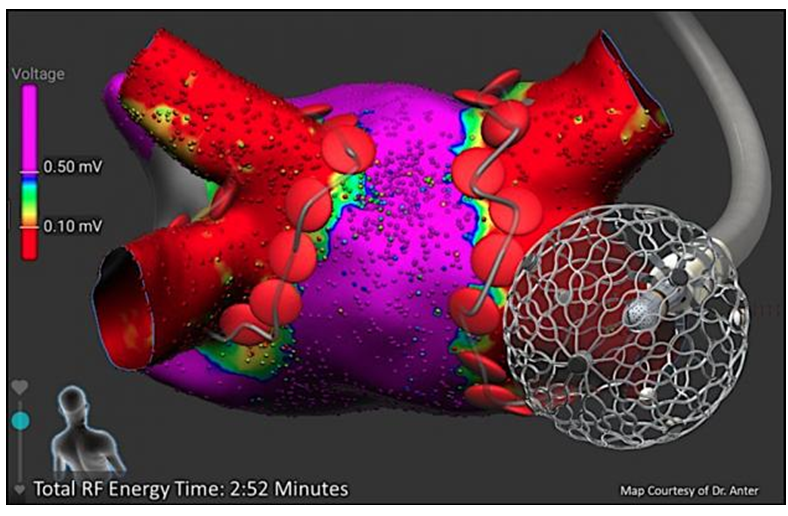
Figure 2: total RF energy time
Source: (Pothineni et al., 2020)
Stent placement: in this phase, doctors elaborate a small metal mesh coil or tube at the end of the catheter inside that facilitates keeping the artery open.
Fractional flow reserve: this technique is known as a pressure management technique that is used in the process of catheterization that is facilitated to see how much blockage there is.
Intravascular ultrasound: this test is done by using the computer and using the transducer those waves from ultrasound in the form of a sound wave that framed an image of the blood flow at the blood vessels. by utilizing the IVUS, doctors are able to see inside the heart and measure the inside of blood vessels.
Catheter ablation is a drug-free technique that is used for a wide range of abnormal heart diseases and heart rhythms also known as arrhythmias (Safavi-Naeini and Rasekh, 2020). The ablation is usually performed when diseases are caused by arrhythmias. It hampers the individual quality of life and hampers therapy job activities, it is an acute form of disorder when the patient has not supposed treatment or by applying for the medicine. It has been measured 90 percent of catheter ablation is successfully administered. It involved thin, flexible tubes that place into the artery in order to reach the target site of the heart. The catheter captured the electrical signals from the activity of the heart and recorded the pinpoint where the arrhythmia is coming from.
The cause of arrhythmia is due to the affected site of the heart or it is destroyed by heat radiofrequency ablation or by freezing process cryoablation. This has an impact on the heart such as creating scar tissues, which is not conducted by electrical signals. For many individuals, erythema is regarded as paroxysmal that is generally known for comes and goes and that signal often captures at the ECG which is difficult to record.
The concepts of AF “Rate Control” and “Rhythm Control” in AF catheter ablation
The two main purposes for managing artery fibrillation such as rate control, and rhythm control.
Rate control
Rate control is associated with the disease of atrial fibrillation. The aim of the rate control is to reduce the symptoms that combine with the heart disease that is associated with excessive rates of heart that prevent the tachycardia that is associated with cardiomyopathy (Sohns et al., 2020). Rate of control added the use of drugs that were associated with negative chronotropic drugs or the intervention of electrocardiogram as well as surgical inventions. Such drugs help to reduce the rate of ventricular that is often found in many individuals’ patients that are associated with atrial fibrillation. If the artery is continued to fibrillate this is regarded as a potential treatment process that helps to improve the symptoms as well as reduce the heart-associated disease. After administering antithrombotic drugs, it helps to reduce the chances of stroke as well as thrombosis. Many researchers found that the actual rate of the optimal heart is currently not known. And the adequate rate of martial fibrillation or ventricular responses beats between 60 to 80 beats per minute. The current study suggests that for the patient who has been suffering from atrial fibrillation the heart rate is reduced by less than 90 beats per minute. Although it has been found no acute drug has been found to reduce the all then associates cardiovascular disease any such recommendation may be flawed. Few data have been gathered in order to reduce cardiovascular disease for the assessment of rate control.
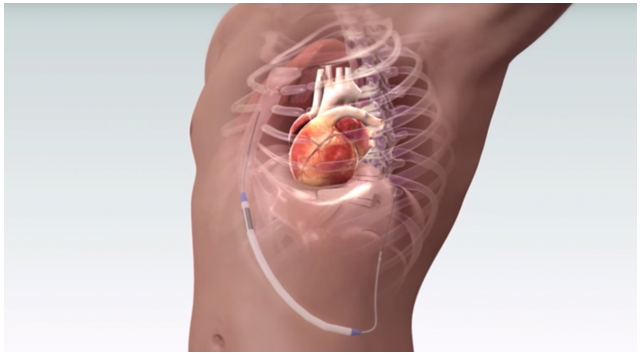
Figure 3: Rate control
Source: (Sugumar et al., 2020)
Rhythm control
There were many ways between rate control and rhythm control, as it has many conditions that are the best approach for the treatment of cardiovascular disease. The involvement of rhythm control is on the insertion of cardioversion or electrophysiological intervention that is associated with cardiovascular diseases that’s converter arrhythmia associated with the disease. Patients were successfully administered with the drug known as antiarrhythmic drugs (Mouselimis et al., 2020). The rhythm control is regarded as sinus control that is successfully associated with the thermic control of the long-term help that helps to reduce or recurrence of cardiovascular disease by helping to the rhythmic control. After the successful administration of rhythmic control that portrays cardiovascular diseases, it reduces the mortality rate and chances of heart failure. On the other hand, the rate of hospitalization is in the adverse effect of treatment with a high amount of drugs that result inconsistent with the general approach of such drugs that are able to reduce cardiovascular disease. The pathophysiology of martial fibrillation is involved with the interaction among the interaction triggers that have been framed in the form of the quick-firing of ectopic loci that is present inside the pulmonary veins and the substrate of atrial tissues which is capable to maintain the arrhythmia. On the other hand, it reduces the chances of stroke among young people. The chances of stroke and thromboembolic events that are reduced by the rhythm control that is related to the lack of appropriate antithrombotic events. Martial fibrillation is mostly associated with heart failure to the presence of abnormalities inside the heart muscle that cause rhythmic abnormalities. It is most common in the adult person that leads to heart failure.
Ablation techniques for the treatment of AF
Over the past several years, catheter ablation of atrial fibrillation has advances that lead to cure such disease as well as cure another disease (Gilbert et al., 2020). Several techniques have been used, among them; three is the technique in order to reduce the disease, such as radiofrequency, cryoablation, and high intensity of focused ultrasound. These are three basic techniques that are used to treat the AF. Among them, radiofrequency can able produce deeper lesions that are used to treat AF as well as cardiovascular disease. This technique used to started cardiovascular disease in an efficient manner on the other hand involves fewer risks in order to treat the disease. Radiofrequency
Radiofrequency is the most general form of energy that is used to treat cardiovascular disease as well as atrial fibrillation. This process is safe to use and consists of an efficacy rate. It has an alternating current that is able to provide a current cycle with a high frequency that is mostly associated with distal electrodes (Garg et al., 2020). The high-frequency cycle that penetrates the patient skin reaches the target side of the heart. The energy of radiofrequency is delayed energy for 15 to 60 seconds. The temperature is increased for the penetration of radiofrequency that leads to an increase in temperature with the symptom of impending. The cause of high temperature due to the use of high-density electrodes in a controlled manner. the size of the electrode is 4 to 8 mm. Relying on the characteristics that use an active electrode and that causes intermediary of surface temperature depending on the characteristics of the electrode. The electrode-tissue surface depends on the maximum temperature that causes the interface of electrode-tissue that is limited to the interface and the temperature relies upon between 45 to 60-degree centigrade. Active electrode confronts a higher electrode that leads to a higher expectation level that is delivered to set between 20 to 60 watts. Catheters that comprise 4 mm of the distal diameter create average deliberation of lesson from 4 to 6 mm diameter and the depth of incision is 2 to the 3-millimeter cube.
The acute lesions produced by radiofrequency apply with the cost of the central segment of coagulation that is surrounded by the consistency of the zone of inflation. On the other bandit continues to monitor the temperature that helps to prevent the chronic cardiovascular disease that is applied on the cardiac tissue that allows greater radiofrequency that is required to input energy with then Ceasar frames deeper lesions.
Cryoablation
Cryoablation is the technique that is used for medication. In this medication, the process uses extreme cold in order to destroy tissue (Romero et al., 2021). By using extreme cold to destroy tissues inside the heat. Doctors use the treatment in order to destroy diseased muscle inside the heart. Doctors prescribed hollow needles or cryoprobes that are cold and thermally conductive. Cryoablation is implemented at the target site of the heat which is positioned adjacent to the heart and the freezing process kills all the tissue inside the heart. Once the probes are placed at the point of the target site and destroy the diseased tissue. After attaching with the target site it is linked with the cryogenic freezing until it removes heat from the cryogenic tip of the probe and the extension of the associated tissues. Ablation occurs at the tissues that have been frozen by using the three mechanisms. The first step is the formation of an ice crystal. By using these steps the cells are disrupted by extreme cold by dismantling the cell membrane and interpreting the mechanism inside the cells. After that blood coagulation stalled the flow of blood to the tissue level and as a result causes ischemia and it leads to apoptosis or cell death. The apoptosis in tissue cells or also known as programmed cell death or cell cascade. The most common application of cryoablation is heart disease (Kautzner et al., 2021). Cryoablation is mainly used for the restoration of cardiac response. It solves the destroyed electrical response to normal electrical response. It freezes the cardiac tissue or the artery and the pathway of the heart that interfaces the normal activities of the heart. The catheter is a very thin tube that is inserted into the vein of the heart in the patient’s leg that is an interesting thread inside the vein where it delivers energy in order to treat the patient’s arrhythmia.
High intensity focused ultrasound (HIFU)
High-frequency focused ultrasound is a therapeutic technique. It is a non-invasive technique that is used to treat cardiac disease. This techne uses non-ionized ultrasound waves that use heart or ablate tissue (Sohns et al., 2020). HIFU is used to facilitate the flow of blood in the blood veins at the lymph. The diseased tissue such as myocardial tissue by using thermal or mechanical processes in order to destroy tissue. It is a prevalent low-cost method that is used to treat myocardial disease. HIFU has been subjected to numerous changes and it gradually develops by undergoing research. This technology is similar to ultrasound imaging. But in this process, it used low frequency and continuous methods in order to treat the disease. Pulse waves have been used in order to reach the thermal activity and reach the desired thermal activity. Acoustic lenses often use in order to reach the desired intensity at the state at the site of the heart. An analogy is to use the magnifying glass in order to reach the target thermal activity in order to destroy the damaged tissue. Using the therapeutic ultrasound set no boundaries in the form of therapeutic ultrasound. It uses lower intensity for their epilation occupational therapy and physical therapy. HIFU is used at the non-invasive heat tissue without cutting the tissue or using the process of an incision. HIFU beams precisely focused that are segmented into the small region of the discarded tissue. It locally assembles a high level of energy. This monkey focuses on the effect of a transducer that emits an ultra high sound that pressure to deliver hog conductive wave and dest not left any unwanted damages to surrounding tissue.
Commercially available device
The most existing commercially available device is cryotherapy. Cryotherapy is an imaging device that is used to treat disease. It is a needle-like applicator that is known as a cryoprobe. This technique uses liquid nitrogen or argon gas that creates deep cold that crafty freezing constitution and destroy the diseased tissue. It also treats cancer cells. This therapy is instructed by a doctor that used to treat atrial fibrillation. Cryogenic therapy is also known as cryosurgery or also known as cryoablation (Nabutovsky et al., 2021). It is quite cost-effective and it is a minimally invasive treatment that uses extreme cold conditions for treating cardiac disease. Cryotherapy or cryoablation used interchangeable terms also known as cryosurgery. This is an open and surgical method. Liquid nitrogen used and high-pressure argon has been used for treating the damaging disease. It creates intense cold in place of the temperature that cured the diseased tissue. There are several surgical problems that have been created during the treatment of cryoablation. In the catheter-based procedure, it is a technique of healing that uses freezing temperature and many recommend cryoablation as its efficacy rate is very high and cost-effective. During the course of heart surgery, it was used as a secondary procedure for treating arrhythmia. This process is undergone during open-heart surgery and used during mitral valve repairs and coronary artery bypass grafting.
American society for aesthetic plastic surgery recommends HIFU as the potential nonsurgical alternative for the benefit of curing disease and it has been seen a huge increase in popularity within the few years after the emergence of this technique. From 2012 to 2017 the total number of procedures has been preferred and increased up to 65 percent. There are several benefits of the utilization of HIFU such as reduction of wrinkles, and also help to bring smoothness to the skin. HIFU is non-invasive and has no inclusion and the average cost of HIFU is 1707 dollars and it takes less recovery time and the risk associated with this is mild redness and tissue swelling. The efficacy of HIFU is high. The study has suggested that 94 percent of people show less effect rate and the rate of imprisonment is higher than other techniques. On the other hand, it has long-term effects, the treatment is persistent for at least six months and it will likely improve the patient in an efficient manner (Bhardwaj et al., 2020). HIFU uses a natural aging process that takes over less time. The drastic dissimilarities of the average cost of HIFU treatment of 7562 dollars. At last, the cost completely relies on the demographic structure and geographical position of that summed number of sessions required to achieve the expected results.
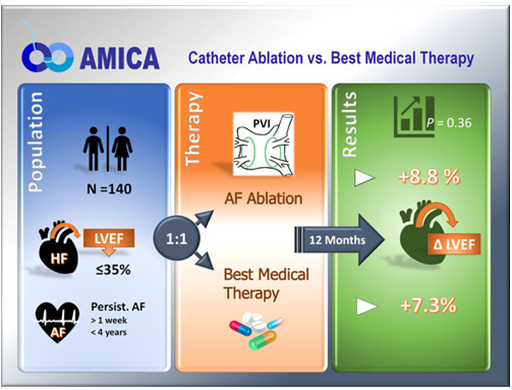
Figure 4: cost comparison
Source: (Arunachalam et al., 2020)
Conclusion
Catheter ablation is a well-known process and it is used to treat cardiac disease. It is a well-established treatment that opened wide options for treating diseases. Over the several decades, catheter ablation of martial fibrillation has evolved and it is under the largely experimental procedure and it established therapeutic options for the certain disease. At present time the majority of the catheter ablation technique is dependent on the techniques that target the pulmonary vein. Several considerable pieces of evidence have been found that catheter ablation providers better symptomatic control for patients and provide patients quality of life. Therefore it is a developer treatment process and it uses the cost-effective technique for catheter ablation. This conclusion is precisely for the patients who have been suffering from cardiac disease. Three treaty mechanisms such as radiofrequency, cryoablation, and high intensity of focused ultrasound used for treating disease. Among them, HIFU is the best approach for treating disease and it is cost-effective.
Reference
Ahn, J.H., Park, J., Jo, J.S., Lee, S.H., On, Y.K., Park, K.M., Oh, E.J., Ko, J.S. and Jeong, J.S., 2021. The frequency of gastroesophageal reflux when radiofrequency catheter ablation procedures for atrial fibrillation under general anesthesia with a supraglottic device: Observational pilot study. Medicine, 100(6).
Arunachalam, K., Maan, A. and Chu, A., 2020. Atrial Fibrillation in Hypertrophic Cardiomyopathy: Evidence-based Review About Mechanism, Complications and Management. Critical pathways in cardiology, 19(2), pp.87-89.
Bhardwaj, R., Neuzil, P., Reddy, V.Y. and Dukkipati, S.R., 2020. Balloon-Based Ablation Technologies. Cardiac Electrophysiology Clinics, 12(2), pp.175-185.
Cha, M.J., Lee, E. and Oh, S., 2020. Zero‐fluoroscopy catheter ablation for atrial fibrillation: a transitional period experience. Journal of arrhythmia, 36(6), pp.1061-1067.
Chen, S., Schmidt, B., Bordignon, S., Tohoku, S. and Chun, K.R., 2020. Pulmonary vein isolation using cryoballoon technique in atrial fibrillation patient after Greenfield vena cava filter implantation. Global Cardiology Science & Practice, 2020(2).
Dretzke, J., Chuchu, N., Agarwal, R., Herd, C., Chua, W., Fabritz, L., Bayliss, S., Kotecha, D., Deeks, J.J., Kirchhof, P. and Takwoingi, Y., 2020. Predicting recurrent atrial fibrillation after catheter ablation: a systematic review of prognostic models. EP Europace, 22(5), pp.748-760.
Garg, J., Shah, K., Turagam, M.K., Janagam, P., Natale, A. and Lakkireddy, D., 2020. Safety and efficacy of catheter ablation for atrial fibrillation in patients with percutaneous atrial septal closure device: Electrophysiology Collaborative Consortium for Meta‐analysis—ELECTRAM Investigators. Journal of Cardiovascular Electrophysiology, 31(9), pp.2328-2334.
Gilbert, B., Balachandar, H., Xue, B., Swanick, J., Santarelli, T., Tibayan, N., Baluyot, E., Fernandes, F. and Malvern, P.A., 2020 Using Simulation to Enhance Existing Methods for Medical Device Training.
Jiang, R., Zei, P.C. and Jiang, C., 2020. Prevention of left atrium esophagus fistula: Appraisal of existing technologies and strategies. Pacing and Clinical Electrophysiology, 43(7), pp.646-654.
Kautzner, J., Albenque, J.P., Natale, A., Maddox, W., Cuoco, F., Neuzil, P., Poty, H., Getman, M.K., Liu, S., Starek, Z. and Dukkipati, S.R., 2021. A Novel Temperature-Controlled Radiofrequency Catheter Ablation System Used to Treat Patients With Paroxysmal Atrial Fibrillation. JACC: Clinical Electrophysiology.
Larson, J., Merchant, F.M., Patel, A., Ndubisi, N.M., Patel, A.M., DeLurgio, D.B., Lloyd, M.S., El‐Chami, M.F., Leon, A.R., Hoskins, M.H. and Keeling, W.B., 2020. Outcomes of convergent atrial fibrillation ablation with continuous rhythm monitoring. Journal of cardiovascular electrophysiology, 31(6), pp.1270-1276.
Mouselimis, D., Tsarouchas, A.S., Pagourelias, E.D., Bakogiannis, C., Theofilogiannakos, E.K., Loutradis, C., Fragakis, N., Vassilikos, V.P. and Papadopoulos, C.E., 2020. Left atrial strain, inter-vendor variability and atrial fibrillation recurrence after catheter ablation: a systematic review and meta-analysis. Hellenic Journal of Cardiology.
Pothineni, N.V.K., Amankwah, N., Santangeli, P., Schaller, R.D., Supple, G.E., Deo, R., Nazarian, S., Garcia, F.C., Dixit, S., Callans, D.J. and Marchlinski, F.E., 2020. Continuous Rhythm Monitoring‐Guided Anticoagulation after Atrial Fibrillation Ablation. Journal of Cardiovascular Electrophysiology.
Romero, J., Gabr, M., Patel, K., Briceno, D., Diaz, J.C., Alviz, I., Trivedi, C., Mohanty, S., Polanco, D., Della Rocca, D.G. and Lakkireddy, D., 2021. Efficacy and safety of left atrial appendage electrical isolation during catheter ablation of atrial fibrillation: an updated meta-analysis. EP Europace, 23(2), pp.226-237.
Safavi-Naeini, P. and Rasekh, A., 2020. Left Atrial Appendage Closure and Pulmonary Vein Isolation. Texas Heart Institute Journal, 47(1), pp.60-62.
Salam, T., Wilson, L., Bohannan, S. and Morin, M., 2020. Safety and Effectiveness of a Novel Fluoroless Transseptal Puncture Technique for Lead-free Catheter Ablation: A Case Series. The Journal of innovations in cardiac rhythm management, 11(4), p.4079.
Skeete, J.R., Du-Fay-de-Lavallaz, J.M., Kenigsberg, D., Macias, C., Winterfield, J.R., Sharma, P.S., Trohman, R.G. and Huang, H.D., 2021. Clinical Applications of Laser Technology: Laser Balloon Ablation in the Management of Atrial Fibrillation. Micromachines, 12(2), p.188.
Sohns, C., Marrouche, N.F., Costard‐Jäckle, A., Sossalla, S., Bergau, L., Schramm, R., Fuchs, U., Omran, H., Rubarth, K., Dumitrescu, D. and Konietschke, F., 2020. Catheter ablation for atrial fibrillation in patients with end‐stage heart failure and eligibility for heart transplantation. ESC Heart Failure.
Steinberg, B.A., Li, Z., O’Brien, E., Pritchard, J., Chew, D.S., Bunch, T.J., Mark, D.B., Nabutovsky, Y., Greiner, M.A. and Piccini, J.P., 2021. Atrial fibrillation burden and heart failure: Data from 39,710 individuals with cardiac implanted electronic devices. Heart rhythm.
Sugumar, H., Nanayakkara, S., Chieng, D., Wong, G.R., Parameswaran, R., Anderson, R.D., Al-Kaisey, A., Nalliah, C.J., Azzopardi, S., Prabhu, S. and Voskoboinik, A., 2020. Arrhythmia recurrence is more common in females undergoing multiple catheter ablation procedures for persistent atrial fibrillation: Time to close the gender gap. Heart rhythm, 17(5), pp.692-698.
Sugumar, H., Prabhu, S., Costello, B., Chieng, D., Azzopardi, S., Voskoboinik, A., Parameswaran, R., Wong, G.R., Anderson, R., Al-Kaisey, A.M. and Ling, L.H., 2020. Catheter Ablation Versus Medication in Atrial Fibrillation and Systolic Dysfunction: Late Outcomes of CAMERA-MRI Study. Clinical Electrophysiology, 6(13), pp.1721-1731.
Wada, T., Sakuragi, S., Saito, T., Kawaguchi, T., Kodera, N., Iida, T., Yamada, T., Nakashima, M., Koide, Y., Kawamoto, K. and Tanakaya, M., 2020. Favorable effect of catheter ablation on nocturnal hypertension in patients with paroxysmal atrial fibrillation. Journal of hypertension, 38(6), pp.1174-1182.

