IMPACTS OF NEW PACEMAKER TECHNOLOGY
The pacemaker is a small medical device that is used to place in the middle part of the chest for the patient those are suffering from the critical cardiovascular disorder. In general, it is an artificial system of the heart that uses an electrical pulse to control the normal rate of the heartbeat in the case of a patient who is suffering from arrhythmias. It can be observed that most of the cardiac patients need to diagnose with the help of an MRI (Magnetic Resonance Imaging) technique which may affect the device. Therefore a new pacemaker technology has been introduced that will help to reduce all these problems. The study will discuss the details of the impact of new pacemaker technology to the patient suffering from the critical cardiovascular disorder.
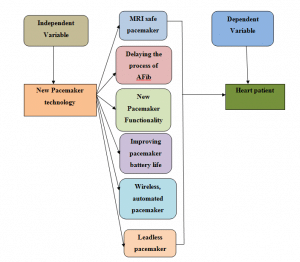
Figure 1: Conceptual framework
3. Concept of new pacemaker technology
Pacemakers are electronic devices that are installed in the heart of the heart patients in order to control the abnormal hearths functions. In addition, the new pacemaker technology has implemented innovative techniques and improved technology which helps the patients in controlling their heart functions more efficiently. However, the innovation and improved new pacemaker technology is a great success and discoveries of the medical sciences and engineering. According to the view of McCauley & Chu, (2017) the new pacemaker technology ensures safe MRI, Delaying AFib, great functionality, improved battery life and automotive and wireless control.

Figure 2: New pacemaker technology
(Source: Omdahl et al, 2016)
The new technology which has been implemented in the pacemakers has the functions of safe MRI. Safety during MRI is very important in order to ensure the safety of the patients during the scanning process. The MRI clear model of the new pacemakers has been introduced by the FDA (Food and Drug Administration) of the United States (Omdahl et al, 2016).
The new technology of the pacemakers provides great and the most appropriate functionality. The functionality of the new pacemaker’s technology includes the proper controls on the abnormal rhythms of the heart and it also controls the heartbeat rates. The new pacemakers technology ensure the prevention of heart attacks and any kinds of disturbances in breathing and blood pumping process of the patients of all age groups.
The new pacemakers’ technology ensures the long life of the batteries and the most improved services. As per the view of Lamiraud & Lhuillery (2016), the new pacemaker’s technology ensures the battery span of 10 to 12 years which is a very long battery life. Along with the long battery life, the new technology of the pacemakers also includes the automotive and wireless controls of the devices which are a major contribution to cardiology development. The automotive controls of the pacemakers accordingly with the body function and age categories are very necessary in order to ensure the health and fitness of the global patients.
4. Concept of the condition of the cardiac patient
The concept of the condition of the cardiac patients can be simply defined as the abnormal and inappropriate function of the hearts. However, the conditions of the cardiac patients are very sensitive in nature and it can cause a number of different diseases and health issues in the person.
The cardiac patients need special medical as well as emotional attention for their survival and well being. As per the view of Beurskens et al (2018) the cardiac patients of the world can suffer from different kinds of heart disease and problems. The most common cardiac problems are congenital heart disease, coronary artery disease, heart failure, mitral regurgitation, and myocardial infarction. All the heart disease greatly affects the health of the patients; the medical attention is needed from the initial stages of the occurrences of the problem. In addition, the cardiac patients also needed more emotional attention for wellness and recovery. The medical sciences and engineering have discovered a number of innovative solutions for the cardiac patients of the world (Boriani et al, 2018). The cardiac patients must avoid high sugar contamination and fat contains food in order to keep their body light. Along with the foods, the cardiac patients must avoid excessive physical works and activities in order to minimize their hearts beats rates.
The causes of the cardiac problems are many; some of the common causes of these problems are the excessive smoking, diabetes, high blood pressure, consumption of drugs and excessive stress. According to Leier, (2017), the cardiac problems of the different patients can be controlled and recover through a different process. Some can be cured by regular treatments and medicines while some patients need pacemakers and other transplants for their survivals. Implementations of the pacemakers are the most effective ways of controlling the cardiac actions of global heart patients.
5. Factors of pacemaker technology
New pacemaker technology has been introduced as the supplement of the old pacemaker technology. It can be observed that the patient suffering from arrhythmias, used to operate and to place the device in the middle of the chest or in the abdomen portion. This acts as the artificial heart in the human body that used to generate an electric pulse and this electric pulse helps to control the normal rate of the heartbeat. As argued by Hinojos & Ilg, (2017), it can be observed that cardiac patient needs to undergo MRI in order to check the condition of their heart. Previously, magnetic resonance creates a problem for the device and thus new pacemaker technology has been introduced in the market.
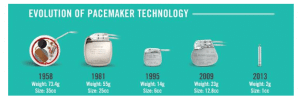
Figure 3: Evolution of pacemaker technology
(Source: Hinojos & Ilg, 2017)
It can be observed that the patient suffering from severe cardiovascular disorder needs to diagnose regularly and also need the image with the help of an MRI device after the implantation of the device. In order to overcome this problem, Biotronik, one of the most famous companies in United States start to design the pacemaker which is appropriate for the MRI performance. The company has incorporated ProMRI technology in the device that used to provide an extra advantage for performing MRI without any hamper. As per the view of Varady, Ostroff & Jacobson, (2016), it was clearly observed that this device incorporates the Accolade MRI, Essentio MRI pacemakers and also new Ingevity MRI pacing lead. This helps the patient to get the complete image via the MRI scanning method under 1.5 Tesla environments.
5.2 Delaying the process of AFib with the help of Antitychardia Pacing
New pacemaker technology has been provided the chance to delay the progression of atrial fibrillation (AF) for the patient suffering from bradycardia. A new algorithm system called ATP (Medtronic’s Reactive Antitachycardia Pacing) has been introduced in the pacemaker system that provides the facility to reduce the progression of atrial fibrillation and can restore the heart to be back in the normal rate (Jacobson, 2016). It also plays a major part in controlling the disease by the termination of Atrial tachycardia.
5.3 New Pacemaker Functionality
New pacemaker technology has some important functionality that helps to improve the condition of the cardiac patient as compared to the previous condition. On the one side, it provides the chance to get the idea about the earlier intervention and on the other it also provides the general concept about the patient suffering from atrial fibrillation. According to Omdahl et al., (2016), it provides the chance to get the concept about the AT/AF status of the patient and also make a clear idea about treatment that is required to provide the AF patient.
5.4 Improving pacemaker battery life
It can be observed that many young people are also suffering from severe cardiovascular disorder and therefore they also need to implement the pacemaker. As a result of this, the battery life for a pacemaker is one of the major points that need to pay more concentration. As per Omdahl et al., (2016), it can be observed that in order to change the battery of the pacemaker, the patients need to undergo serious surgery. Therefore, in this technology, scientists have enhanced the longevity of the battery about 12.1 years in order to save the patient from critical surgery.
5.5 Wireless, automated pacemaker monitoring
The new pacemaker technology provides the chance to use the wireless and automated pacemaker in order to monitor the patient’s health condition. In this method, the physicians can diagnose the patient face to face and can make them alert about any serious issues (Leier, 2017). This allows the daily monitoring system and also a thorough analysis of the health status of the patient.
It can be observed that in the case of an electronic pacemaker, lead helps to make the connection with the heart and the device in the patient’s body. As argued by Boriani et al., (2018), lead is one of the weakest components that may lead to ICD (Implantable Cardioverter Defibrillator) or sometimes it may cause some infections due to the lead.
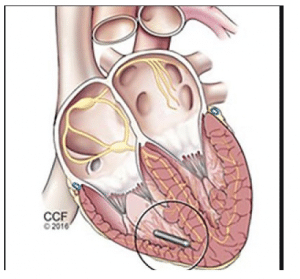
Figure 4: Leadless pacemaker
(Source: Boriani et al., 2018)
This technology allows us to generate the pacemaker without lead and thus helps to reduce the infection. Along with this, it has also reduced the cost of operation, the risk of infection while performing the surgery due to the installation of lead.
6. Advantages and disadvantages of new pacemaker technology
There are several advantages and disadvantages of new pacemaker technology, which are as follows-
Advantages:
- It provides an MRI safe imaging that helps the patient to undergo the MRI without the fear of any damage to the device.
- It saves the cost of surgery and also the risk of complicated surgery methods by installing the leadless pacemaker (Beurskens et al., 2018).
Disadvantages:
- As this technology has been newly introduced in the market, more researches need to perform, to evaluate the risk factors of this system. Along with this, the physicians need to be properly trained in order to perform the surgery and to place the device in the patient’s body.
- The main limitation of the system is that the scientists are unable to place the atrial pacing or the dual-chamber pacing in the device (Lamiraud & Lhuillery, 2016).
7. Problems related to the previous pacemaker technology
The pacemaker is considered the artificial heart that helps to control the normal rhythm of the heart in the case of the severely affected patients. From the view of Lee, Mulpuru, & Shen, (2018), it can be observed that the patients who are suffering from the slow rate of the heartbeat as compared to the normal pulse rate. It can be found that the abnormal condition of the heart may result in the breathlessness; improper functioning of the heart or even it may result in the dearth of the patient. In such cases, the pacemaker is generally placed in the middle of the chest or in the abdomen part in order to maintain the normal beat of the heart. As argued by Leier, (2017), pacemaker technology provides both positive and negative effects on the patient. The negative effect caused due to the pacemaker technology is as follows-
- Lead dislodgement: in the case of a pacemaker, the lead helps to connect with the heart and the device and thus it controls the normal rhythm of the patient’s heartbeat. As argued by Oliveira, (2018), it can be clearly observed that the deposition of lead in the body results in severe complications for some cases of the patient. It can be observed that lead may get dislodged from the chamber or within the chamber and thus it creates severe problems.
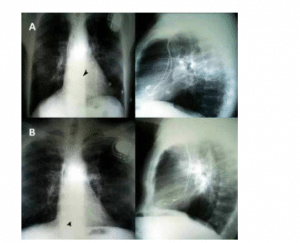
Figure 5: Lead dislodgement
(Source: Oliveira, 2018)
Along with this, another major issue is that the dislodgement can only be observed by the radio graphical imaging and it is very difficult to sense. On the other hand, the only method to restore the lead content is by surgery which is much-complicated and costly too. As a result of this, this creates a severe problem for the cardiac patient after the implantation of the pacemaker.
- Implantation of pacemaker sometimes results in severe bleeding or the appearance of bruises in the place where the doctors have done the surgery (Sebastian & Jose, 2017).
- A pacemaker is an electrical device therefore after implantation of a pacemaker; it is difficult to perform MR Imaging of the heart patient. As per Yan et al, (2018), MR Imaging is one of the important parts in order to get the idea of the heart condition after the operation.
- The implantation of pacemaker results in the pneumothorax which is defined as the collapsed lung. It can be observed that the patient with a pacemaker may feel breathing problems or chest pain due to this condition. According to Zhao et al, (2018), in this method, the air starts to leak and start to push in the space between the wall of the chest and the lungs. As a result of this, the patient used to feel the pain in the chest and thus it creates severe issues.
8. Effects of new pacemaker technology on the cardiac patient
As per the discussion, it can be clearly observed that pacemaker technology results in many problems for the cardiac patient. On the one side, as per Zhao et al., (2018), it results in the pain in the chest, high bleeding or the formation of the bruises in the part of the surgery. Along with this, it also results in serious and complicated infections due to the lead discharge within or outside the chamber. On the other side, this technology also provides a positive impact on cardiac patients as it provides the chance to control the normal beating of the heart. As a result of this, this technology also saves the patient from death.
As a result of this, scientists are paying more attention to the improvement of pacemaker technology in order to improve the condition of the heart patient. The advancement of the new technology has resulted in the formation of a lead-free pacemaker and also MRI free pacemaker so that it can stand against the infection caused due to the lead. It also enables the chance to get the image with the help of MRI and thus it helps to reduce the suffering of the patient. As argued by Watanabe et al., (2016), it is also important to look for the side effects of the new technology and the method to reduce the issue.
The whole study has concluded that the pacemaker is very much important for the cardiac patient but it has also resulted in some complications for the patient. The new pacemaker technology has been introduced in order to resolve the complication due to the old method. It can be observed that new pacemaker technology provides the chance to get an MRI without any problems with the device. Along with this, it also reduces the chance of getting an infection due to the lead. The wireless pacemaker has been made possible to diagnose the patient very easily and efficiently. Along with this, it is also important to pay more attention to the side effects of the new pacemaker technology and need to research the methods to reduce the issue.
Beurskens, N. E. G., Tjong, F. V. Y., Neuzil, P., Defaye, P., Delnoy, P. P., Ip, J., … & Exner, D. (2018). P3872 The learning curve associated with the implantation of the nanostim leadless cardiac pacemaker. European Heart Journal, 39(suppl_1), ehy563-P3872. Retrieved from: https://academic.oup.com/eurheartj/article-pdf/39/suppl_1/ehy563.P3872/25575246/ehy563.p3872.pdf, [retrieved on: 6th January, 2020].
Boriani, G., Bertini, M., Saporito, D., Belotti, G., Quartieri, F., Tomasi, C., … & Diotallevi, P. (2018). Impact of pacemaker longevity on expected device replacement rates: Results from computer simulations based on a multicenter registry (ESSENTIAL). Retrieved from: Clinical cardiology, 41(9), 1185-1191. https://onlinelibrary.wiley.com/doi/pdf/10.1002/clc.23003, [retrieved on: 6th January, 2020].
Hinojos, A., & Ilg, K. (2017). Removal of Misplaced Left Ventricular Single Lead Pacemaker in a Patient Presenting with Recurrent Transient Ischemic Attacks. Spartan Medical Research Journal, 2(1), 6068. Retrieved from: https://smrj.scholasticahq.com/article/6068.pdf, [retrieved on: 6th January, 2020].
Jacobson, P. M. (2016). U.S. Patent No. 9,358,400. Washington, DC: U.S. Patent and Trademark Office. Retrieved from: https://patentimages.storage.googleapis.com/09/de/89/719ddace1db820/US9358400.pdf, [retrieved on: 6th January, 2020].
Lamiraud, K., & Lhuillery, S. (2016). Endogenous technology adoption and medical costs. Health economics, 25(9), 1123-1147. Retrieved from: https://hal-essec.archives-ouvertes.fr/hal-01218064/document, [retrieved on: 6th January, 2020].
Lee, J. Z., Mulpuru, S. K., & Shen, W. K. (2018). Leadless pacemaker: Performance and complications. Trends in cardiovascular medicine, 28(2), 130-141. Retrieved from: https://www.researchgate.net/profile/Justin_Lee16/publication/319020946_Leadless_pacemaker_Performance_and_complications/links/5c82e2e892851c695063f841/Leadless-pacemaker-Performance-and-complications.pdf, [retrieved on: 7th January, 2020].
Leier, M. (2017). Advancements in pacemaker technology: the leadless device. Critical care nurse, 37(2), 58-65. Retrieved from: https://pdfs.semanticscholar.org/543b/39787e24bf019a0246044a045d4c9b976068.pdf, [retrieved on: 6th January, 2020].
McCauley, B. D., & Chu, A. F. (2017). Leadless cardiac pacemakers: the next evolution in pacemaker technology. Rhode Island Medical Journal, 100(11), 31-34. Retrieved from: http://www.rimed.org/rimedicaljournal/2017/11/2017-11-31-cont-mccauley.pdf, [retrieved on: 6th January, 2020].
Oliveira, M. M. (2018). Enhanced pacing modalities in bradycardia patients: Can technology reduce costs?. Retrieved from: https://comum.rcaap.pt/bitstream/10400.26/25643/1/RPC.pdf, [retrieved on: 7th January, 2020].
Omdahl, P., Eggen, M. D., Bonner, M. D., Iaizzo, P. A., & Wika, K. (2016). Right ventricular anatomy can accommodate multiple micra transcatheter pacemakers. Pacing and Clinical Electrophysiology, 39(4), 393-397. Retrieved from: https://onlinelibrary.wiley.com/doi/pdf/10.1111/pace.12804
Sebastian, S., & Jose, N. (2017). Leadless intracardiac transcatheter pacing system. Asian Journal of Nursing Education and Research, 7(1), 133. Retrieved from: https://www.researchgate.net/profile/Neethu_Jose3/publication/316486067_Leadless_Intracardiac_Transcatheter_Pacing_System/links/5978406145851570a1b6b015/Leadless-Intracardiac-Transcatheter-Pacing-System.pdf, [retrieved on: 7th January, 2020].
Varady, E., Ostroff, A., & Jacobson, P. M. (2016). U.S. Patent No. 9,511,236. Washington, DC: U.S. Patent and Trademark Office. Retrieved from: https://patentimages.storage.googleapis.com/a9/4d/fc/37b32d9d2410e4/US9511236.pdf, [retrieved on: 6th January, 2020].
Watanabe, T., Shinoda, Y., Ikeoka, K., Fukuoka, H., & Inui, H. (2016). Pacemaker Lead Perforation during Right Ventricular Outflow Tract Pacing Importance of Heart Rotation at Pacemaker Implantation. J Clin Case Rep, 6(707), 2. Retrieved from: https://pdfs.semanticscholar.org/9c50/fb9d5747ee78a8f7298b535439f5e4c32b0c.pdf, [retrieved on: 7th January, 2020].
Yan, H., Guo, F., Zhu, D., Stryker, S., Trumpore, S., Roberts, K., … & Liu, W. (2018). On the use of bolus for pacemaker dose measurement and reduction in radiation therapy. Journal of applied clinical medical physics, 19(1), 125-131. Retrieved from: https://aapm.onlinelibrary.wiley.com/doi/pdf/10.1002/acm2.12229, [retrieved on: 7th January, 2020].
Zhao, Z. G., Williams, M., Staniloae, C., Vapheas, E., Du, R., Wang, M., … & Hisamoto, K. (2018). TCT-121 A Highly Predictive Model for New Permanent Pacemaker Implantation after Transcatheter Aortic Valve Replacement with Contemporary Self-Expanding Valves: Importance of the Membranous Septum Length. Journal of the American College of Cardiology, 72(13 Supplement), B53. Retrieved from: http://www.onlinejacc.org/content/accj/72/13_Supplement/B53.1.full.pdf, [retrieved on: 7th January, 2020].