BSC Social Work Assignment Sample
Unaccompanied asylum seekers: stressors and resilience faced in the host country.
Introduction
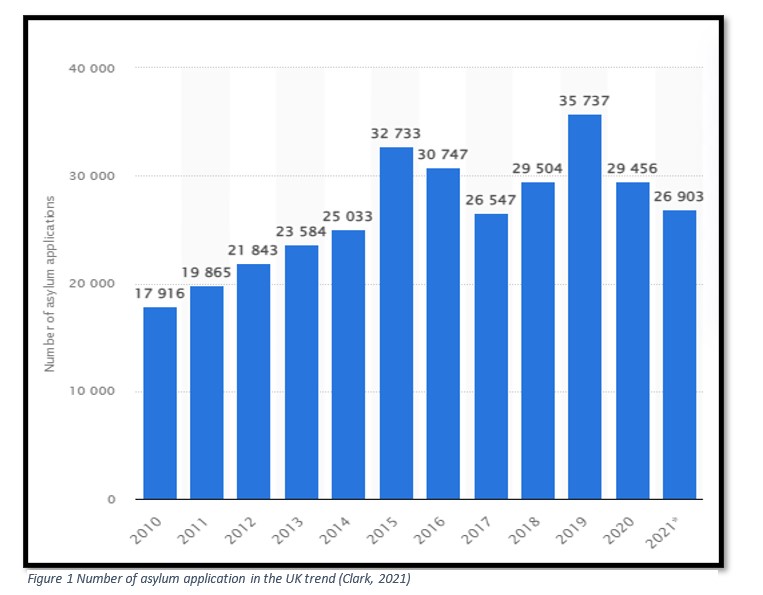
At the end of 2020, there are expected to be roughly 33 million child refugees in the world (UNICEF, 2021). In 2020, the UK received 3,103 asylum requests from unaccompanied minors, a 3% reduction from the previous year (Home Office, 2021); the chart below provides further information of long-term trends:
At its peak in 2016, there were 3,290 unaccompanied children seeking asylum in the United States, a figure that has steadily climbed since then. Although the UASC figures (green line) represent a small percentage of all asylum petitions, they are increasing. The majority of UASCs are between the ages of 16 and 17. (yellow column). UASCs accounted for little over 10% of all asylum applications in the UK in 2018 – a modest but significant share of the total (Home Office, 2019).
Unaccompanied children in the United Kingdom are required to be cared for by the local government under the 1989 Children Act (Johnson, 2020). When a child was brought to a local authority for the first time, that authority was responsible for the child. According to Kent, which houses the port of Dover and is responsible for a considerable number in contrast to other local authorities, this resulted in an imbalance. Local authorities in England had a high concentration of UASCs prior to the national transfer plan in 2015.
When the government implemented the national transfer protocol in 2016, it made it possible for UASCs to be relocated from one local authority to another, where there was more capacity, as an interim transfer protocol. As a point of arrival for a disproportionate number of unaccompanied children, any participating local authority is not expected to bear the burden of providing shelter and care for these children under the national transfer mechanism,” according to government data. There should be no more than 0.07 percent of a local authority’s child population assigned to care for UASC under this programme.
Now that we’ve figured out the political climate in which UASCs are arriving, we need to figure out the internal and external forces influencing these newcomers. Refugees and asylum seekers suffer a wide range of stresses, including as “armed war, the loss or murder of family members, torture, arbitrary detention, and sexual and other types of abuse”, when they arrive in their destination countries (Turrini, et al., 2017). Anxiety, sadness, and post-traumatic stress disorder (PTSD) are all common mental health issues among refugees who have been resettled in the United States (Bogic, et al., 2015; Reavall, et al., 2017). Methodological discrepancies, as well as individual factors and post-migratory stresses, have been found to account for much of the heterogeneity in prevalence rates seen in previous systematic reviews. More than 20% of refugees are estimated to suffer from anxiety, depression, or post-traumatic stress disorder. According to a recent assessment of 42 studies on refugee children, the prevalence of post-traumatic stress disorder (PTSD) ranges from 40 to 63 percent, while the prevalence of depression ranges from 25 to 50 percent (Reavall, et al., 2017).
According to long-term Canadian studies, despite the high rates of pre-migration trauma and considerable psychological challenges, most refugees with a stable status adapt successfully. Refugee pathology may be explained by a literature that emphasises dysfunction and sickness above resilience and post-traumatic growth. Refugees’ well-being, rehabilitation, and mental health challenges are influenced by a wide range of factors, including stress reduction in the post-migratory context, resilience building, and the negative impacts of trauma before to and during migration (Slobodin and de Jong, 2015).
However, among all categories, the UASCs require special attention because of their increased vulnerability and the degree of psychological impact it might have on them (Mitra & Hodes, 2019). UNHCR gives children and adolescents special consideration because of their vulnerability. Hosting countries are obligated to provide UASCs with particular protections, such as proper care and support, education, housing, and legal assistance, to ensure their safety (UNHCR, 2018).
UASCs are seen as a particularly vulnerable population because they are, by definition, not accompanied by parents or other primary caregivers. It’s more likely that they’ve had numerous potentially traumatic situations including abuse, exploitation, and the loss of family members than unaccompanied kids and non-immigrants (Fazel et al., 2015). After surviving a series of horrific events, including having their academic and social lives disrupted, they are then forced to travel to a new nation and learn a new language and adapt to a new culture (El Baba & Colucci, 2018). High degrees of psychological discomfort and an elevated risk of mental illness are linked to such traumatic experiences in one’s life’s past (El Baba & Colucci, 2018).
A comparative group of UASC and their accompanying counterparts has not been examined to see if the UASC had experienced more war trauma in their countries of origin. Travel and arrival in resettlement nations may pose additional risks. This can help alleviate the psychological stress produced by their prior difficulties when they arrive in their new home nations. Family separation and the extent to which a supportive living environment could alleviate the discomfort induced by past traumatic events are unknown. An important feature of public mental health in light of the huge number of people in England who live on their own and have no help is this.
The specific aims of this study were to investigate, first, whether UASC had experienced a higher level of past adversities and war trauma than accompanied asylum-seeking and refugee children (ARC) and how they could act as additional stressors, and second, whether the UASC had higher levels of psychological distress. The third aim was to identify policy directives that could be developed as a result of this review.
Methodology
Definitions
Asylum Seeker: Someone who has filed for asylum outside of their country of origin and is now awaiting a response to their application is referred to as an asylum seeker. The applicant has made an official request to be recognised as a refugee. “Asylum seekers” is a word that the Refugee Council considers “dehumanising,” and prefers the term “person seeking asylum.”
Child/Children: Instead of using the terms “young person” or “young people,” I use the phrase “child” or “children” when discussing “individuals under the age of 18 years old,” which is a legally defined group.
Refugee: The 1951 United Nations Convention Relating to the Status of Refugees defines a refugee as:
“A person who owing to a well-founded fear of being persecuted for reasons of race, religion, nationality, membership of a particular social group or political opinion, is outside the country of his nationality and is unable or, owing to such fear, is unwilling to avail himself of the protection of that country; or who, not having a nationality and being outside the country of his former habitual residence as a result of such events, is unable or, owing to such fear, is unwilling to return to it.”
UASC/ Unaccompanied minor: According to the Home Office, a UASC is someone who is “under the age of 18 or who appears to be under the age of that age, in the absence of documentary evidence establishing age,” and who “is applying for asylum in their own right; and who has been separated from both parents and not being cared for by an adult who by law or custom has the responsibility to do so.”
Search Strategy
For the search, two repositories like Google Scholar, Elsevier, NCBI and PUBMED were searched using the keywords: UASC, asylum, stressors, Unaccompanied minor, refugee, distress, asylum seeker. The results obtained were then filtered based on various criteria. First the time frame of the papers selected was noted between 2010 and 2021. Then, the abstracts of all the papers were manually reviewed to identify the papers that most suited the needs of the project at hand. Following PRISMA’s recommended reporting items, a comprehensive literature search is conducted to identify any relevant studies. We searched MEDLINE, PUBMED, and Allied Health Literature to find studies on neck discomfort in cyclists that were descriptive and comparative. Unaccompanied minor, refugee, distress, and asylum seeker were among the terms thrown around. In addition, we checked the citations of current studies on UASCs’ psychological concerns. Asylum seekers’ danger and resilience were the focus of six of the 28 articles we uncovered, all of which dealt with the topic at hand. Google Scholar and the National Institute for Health and Care Excellence were also used to get a better understanding of the subject and lessen the likelihood of bias in published work, respectively. According to the systematic review, only a few studies have dealt with systematic literature reviews in this way. As a result, there is an urgent need to fill a huge void in the literature.
The reference section of this paper will include a list of publications retrieved from various databases and websites. This will make it easier for the reader to locate relevant research papers. The data extraction form prepared for this review will be used to determine the number of articles to be screened. Based on the criteria for inclusion and exclusion, the quality will be evaluated. PRISMA mandates that at least two reviewers be involved in the process. Randomization and allocation concealment are examples of selection bias, while blinding of subjects, assessors, and therapists is an example of performance bias; insufficient outcome data is an example of attrition bias; and selective reporting of results is an example of reporting bias.” The aforementioned potential sources of bias will be examined in each and every study.
Literature review
Impact of the asylum seeking process on stress
Stress is a major repercussion of a dysfunctional asylum system. In Colman’s (2015) definition of stress, ‘psychological and physical strain or tension’ is a ‘physical and emotional strain or tension created by physical, emotional, social, economic, or occupational circumstances’ Whenever a stressor (i.e., something that creates anxiety) triggers a stress reaction, people adopt coping methods to overcome, minimise, or tolerate the discomfort they feel. A coping strategy is an action or thinking that reduces the negative consequences of stress on one’s health and well-being. Asylum seekers have to learn to cope in order to overcome or reject the negative impacts of exile. There are several ways to cope with stress, and one of them is to look for help.
In times of crisis and upheaval, family support is essential for coping (Skinner et al. 2003). For asylum seekers, findings on family support have been equivocal (Schweitzeret al., 2007). Asylum seekers who have been separated from their families or whose relatives have died are obliged to rely less on them for support (Schweitzer, et al., 2007). For example, in situations where a family member is forced to escape their home, sadness or fears for their loved ones can aggravate rather than alleviate the stress. The strain on a relationship that moving and resettlement can cause is another source of stress (Berry 2006).
Additional social support can be found in the form of friends. Asylum seekers gain greatly from the support of those who have experienced similar hardships, particularly through reducing isolation and giving a listening ear (Behnia 2015). A study indicated that sharing experiences with others can help ease the transition to a new country and alleviates the stress of migrating (Liebling et al. 2014). Some studies have indicated that individuals were exploited by their peers when they relied on this type of support (Cuthill, et al., 2013). As a result, the volunteers in these research may be at increased risk of being exploited because of their circumstances (Crawley, et al., 2011). Fear and distress in individuals who remain after their friends were deported was discovered to be another harmful effect of friendships (Liebling et al. 2014).
Third-sector organisations might also be accessed for assistance in coping. Some studies have indicated that these services are useful in providing practical aid, but fall short in their assistance with asylum requests (Cuthill, Siddiq Abdalla, and Bashir 2013). According to other studies, asylum seekers are reluctant to seek help from social service agencies out of a sense of distrust and apprehension that it may hurt their asylum case (Rider 2014).
Resilience among unaccompanied asylum seekers
Following trauma or psychosocial adversity, children and adolescents tend to have a positive adjustment process. This is despite the increased risk of mental health disorders. Resilience is a study concept that emphasises positive results despite high risks or unfavourable expectations (Keles et al., 2018). For the past 40 years, developmental scientists have been puzzled by the topic of why some children and teens have difficulty adjusting while others are able to cope with similar life challenges (Garmezy, et al., 1984). People that study the attribute think of it as an indicator of long-term health and well-being (Bonanno, 2004). It has also been characterised as a dynamic process that results in constructive adaptation in the face of considerable adversity. In spite of momentary decreases in mental, cognitive, and social functioning as a result of life’s ups and downs, resilient children and teens often bounce back and resume normal functioning (Luthar, 2006).
Contextual factors may influence the resilience process, which may result in distinct developmental paths for different youth subgroups (Hodes et al., 2008). Resilience processes among unaccompanied refugee kids have not been fully explored, despite an increase in use of this paradigm among immigrant and refugee youths in recent years. Individual differences among unaccompanied refugees in terms of risk and protective factors are expected to affect their development outcomes differentially over time.
This group of vulnerable children, both those who are still in the process of applying for asylum and those who have been granted refugee status and are now in the process of being resettled, is challenging to integrate into the resilience paradigm. They’ve all had to deal with the pain of losing or being separated from loved ones. More than seventy-nine percent of them (Oppedal & Idse, 2015) have first-hand knowledge of war and the catastrophic experiences that accompany it. In spite of this, they escaped and travelled long and risky routes and engaged in the resettlement and acculturation process without the help of intimate adult relationships, which is a sign of resilience. Unaccompanied kids have a consistently high risk of mental health disorders, according to longitudinal study, but individual differences over time have been found to be substantial (Keles et al., 2015). According to this, many unaccompanied minors have mental health issues, which suggests that they are clinically vulnerable. For example, a refugee’s pre-migration hardships, as well as their unique experiences upon arrival in the new country, provide a range of possible adjustment paths for refugees.
Stressors and possible mitigation strategies
Many of the refugees studied by Hodes and colleagues in 2010 were from the Balkans and Horn of Africa, where they had been subjected to extreme levels of war trauma and family bereavement. The majority of the UASC were living in foster homes, semi-independent or fully independent arrangements, or were living in their own homes (Cortvriend, 2020). There were many more in the unaccompanied group who were suffering from severe post-traumatic stress symptoms, with more than half of them being at risk of developing PTSD. Posttraumatic stress symptoms in the UASC were shown to be higher among females in both groups, according to a covariance analysis. There was an interesting connection between age and posttraumatic symptoms, with the unaccompanied group experiencing higher symptoms while the accompanied group experienced fewer. For individuals in low-support living circumstances, i.e. those who were living on their own or semi-independently, post-traumatic stress symptoms were more prevalent. In regression analysis, it was discovered that depression symptoms were more common in women, and that the location of origin and kind of living arrangement were important factors.
In the face of suffering and loss, social support, whether from peers or parental figures, serves as a buffer (Demazure et al., 2017). It may be possible for the young people to better articulate their sentiments of despair and hopelessness if they have foster parents or guardians in specific circumstances (Kronick, 2018). A family structure in a foster placement would help the UASCs re-establish a sense of belonging and smooth their transition into the local community, as many of the UASCs have lost attachment figures and other members of their family. Following their arrival in a new nation, many immigrants will continue to be affected by the turbulence caused by social unrest and fears of deportation. Depressive symptoms can be alleviated by socialising with others who share similar backgrounds and possibly similar ages. As a result of the group effect, UASCs are more likely to benefit from the aid they receive from their caretakers. There is a link between higher depressive symptoms and acculturative stress for UASCs who are placed in culturally matched foster families (O’Higgins et al., 2018).
Stress can be lessened if a child has a safe place to call home and can feel the warmth and concern of an adult/carer who cares about him or her. There may be a link between the persistence of internalising symptoms and the stress experienced by UASCs (Vervliet, et al., 2014). A lack of peer support has been identified in several research (Mels et al., 2008), emphasising the importance of caregivers or foster parents. Indeed, for those UASCs that are in communication with their families, this support acts as an antidote to stressful occurrences in their lives (Sierau, et al., 2018).
If UASCs have already had contact with MHS and are able to convey their mental health issues, they may be better able to do so. Post-traumatic stress disorder (PTSD) symptoms and MHS exposure were shown to be unrelated, whereas military service was linked to depressed symptoms. There’s a chance this is due to the referrers’ increased ability to describe or recognise depression symptoms. The United Kingdom study likewise discovered unmet needs, just like the Dutch study.
Although the 2015–2016 European refugee crisis has brought attention to this issue, screening and early diagnosis of psychological distress amongst UASCs has been lacking (Fegert, et al., 2018). Self-report tools, such as the Strengths and Difficulties Questionnaire (Goodman, et al., 2000) used by social workers in the UK for UASCs (Goodman & Goodman, 2012), may have inadequate sensitivity for diagnosing depression, anxiety disorders, and PTSD in routine practise. As a result of better screening, the most vulnerable UASCs could be more quickly sent to specialists for appropriate care.
There are many reasons why UASCs may be reluctant to accept support from adults, even if they are offered MHS. In their home countries and on their voyage, many would have experienced traumatic experiences perpetrated by adults, such as smugglers, traffickers, and custom authorities. They may have a hard time trusting someone they don’t know. Fear of jeopardising their chances of receiving refuge may also be a barrier to seeking and receiving treatment from MHS. PTSD may also be linked to a fear of disclosure, which could explain some of the avoidance that people with PTSD exhibit.
UASCs from countries with little or no MHS provision may not be aware that certain interventions and specialists, such as psychologists and therapists, exist because of language and cultural differences. It is also possible that local children and adolescents are unaware of the resources that exist, so even if they are disturbed, they may not be able to articulate this or have the information necessary to request assistance.
Coping mechanisms in use
The most common method of coping with the anxiety brought on by the asylum process was to engage in mindless activities such as television watching or playing video games. It is common for people to use distraction as a way to cope with stressful situations by engaging in a wide range of activities (Skinner et al. 2003). To keep their minds off their situation at home, male asylum seekers engage in activities outside the house, according to studies (Renner and Salem 2009). Additionally, these strategies fulfil the desire to be useful and to retain one’s masculinity, which is a primary source of stress relief (Cuthill, et al. 2013). To reduce stress, Laban (2015) argues that it is not only about engaging in activities but also about interacting with others and breaking out of one’s isolation.
Many asylum seekers (Cuthill, et al. 2013) regard employment as an important component of their identity, and volunteer work can help them keep that portion of their identity intact. According to Gower (2016), enabling asylum seekers to work would alleviate the detrimental effects on mental health and self-esteem that come with being shut out of the labour market for an extended period.
Family is commonly regarded as a reliable source of support in the coping literature as a whole (Skinner et al. 2003). Even while the asylum procedure is stressful for all members of a family, asylum policy also produces an environment that supports maladaptive coping behaviours.
Reassessing stress or their position was one of the ways asylum seekers utilised internal coping mechanisms. Comparing the present or future to the past or future was another common method. It is a type of coping strategy in which an individual deliberately alters their perception of an unpleasant event in order to see it as an opportunity for growth (Skinner et al. 2003). A cognitive reappraisal technique is cultural distancing, a strategy in which asylum seekers favour their own ancestry while separating themselves from the culture of their new home (Doggett 2012). Rather than focusing on the negative features of their home country, people focus on the positive parts, allowing them to retain their cultural identity and lessen emotions of displacement and disorientation (Doggett 2012). When people choose to remove themselves from their culture, they may instead see their current circumstance as a great opportunity to grow and improve themselves (Abi-Hashem 2006). When people compare themselves to those who are worse off, they tend to feel better about their own status (Cuthill, et al., 2013).
Support systems for asylum seekers with mental health problems
Access to specialised mental health services has been studied in four separate studies (MHS). When it comes to mental health services, only 12.7 percent of UASCs had sought help, according to a research by Bean et al. (2006). A closer look revealed that just 30% of UASCs had their emotional discomfort recognised by their parents or teachers. Bean et al. (2008) observed that there was little association between a student’s self-assessment of need for MHS and a guardian/report. teacher’s
Only 17% of UASCs had MHS interaction in the study conducted in England (SanchezCao, Kramer, & Hodes, 2013). For any psychiatric disease, UASCs who had contact with services were more likely to score in the abnormal range of self-reported SDQ scores than those who did not (6.7 percent). MHS contact was more common among UASCs at high risk for depression (41.6 percent) than those at low risk (40.7 percent) (6.7 percent).
MHS referrals in England were studied in another study (Michelson and Sclare 2009). Referrals from social service organisations were more common for UASCs, whereas GP referrals were more common for those who accompanied their parents. According to MHS utilisation, there was a greater percentage of unaccompanied adolescents who skipped appointments (33%), almost double the rate of accompanying minors who missed appointments (12%). UASCs were less likely than accompanied children to have access to and receive trauma-focused psychiatric therapies, despite the fact that UASCs have a higher risk of PTSD. There were also substantial differences between UASCs and non-UASCs when it came to cognitive therapy, anxiety management and parent/caregiver training.
Findings from Landgraf (2008) show that mental health counselling does not improve functional outcomes. The three other studies looked at cognitive behavioural treatment (CBT) for children who have been exposed to violence and war, which has a significant body of work already established (Morina, et al., 2017). Understanding harmful thoughts and behaviours, and establishing personal skills for dealing with stress are key components of the therapy, which is tailored to address the wide range of presentation among the UASC population (Demazure, et al., 2017).
Trauma-focused cognitive behavioural treatment (TF-CBT) has been shown to be beneficial for adolescents with moderate to severe PTSD symptoms, according to a study by Unterhitzenberger et al. (2015) from Germany. Both the Clinician Administered PTSD Scale for Children and Adolescents and the Post-trauma Diagnostic Scale (PDS) were found to be helpful with TF-CBT; improvements were seen. At the completion of the treatment, just one instance still satisfied the DSM-IV criteria for PTSD. Two single-case investigations conducted in the United Kingdom, one by Unterhitzenberger and Rosner (2016) and the other by Vickers (2005), found that TF-CBT dramatically reduced PTSD symptoms.
Discussion
Coping with stress
Asylum inmates are under a lot of stress as a result of a broken system. Psychological and physical strain or tension’ is defined by Colman as ‘physical and emotional strain or tension that arises as a result of a person’s physical and mental conditions’ When confronted with a stressor (i.e., anything that causes anxiety), people often resort to coping mechanisms in order to reduce or eliminate the discomfort they are experiencing. An activity or thought that minimises the negative effects of stress on one’s health and well-being is a coping technique. To overcome or reject the harmful effects of exile, asylum seekers must learn to cope. Looking for help is one method to deal with stress, but there are many more.
The ability to rely on one’s family during times of difficulty is critical to one’s ability to cope (Skinner et al. 2003). Family support for asylum seekers has shown mixed results (Schweitzeret al., 2007). If a family member has died, an asylum seeker must rely less on them for financial assistance (Schweitzer, et al., 2007). A family member’s sadness or anxiety for loved ones might exacerbate rather than reduce the stress in circumstances where a family member is forced to leave their home. Another form of stress is the pressure on a relationship that relocating and resettlement can have on a family (Berry 2006).
Friends can be a source of additional social assistance. Asylum seekers benefit enormously from the assistance of those who have been through similar circumstances, especially through reducing isolation and providing a listening ear (Behnia 2015). The stress of moving to a new nation can be reduced by exchanging experiences with others, according to a study (Liebling et al. 2014). Some studies have shown that those who rely on this form of support are exploited by their peers (Cuthill, et al., 2013). Thus, participants may be more vulnerable to being exploited because of their unique situations in these studies (Crawley, et al., 2011). Another detrimental effect of friendships was shown to be fear and distress in those who remained after their friends were deported (Liebling et al. 2014).
It is also possible to seek help from third-party organisations. Some studies have found that these programmes are useful in providing practical assistance, but they fall short in their assistance with requesting asylum (Cuthill, Siddiq Abdalla, and Bashir 2013). Asylum seekers, according to other research, are reluctant to seek assistance from social service providers because they are afraid that doing so may harm their asylum application (Rider 2014).
Addressing mental health issues through preventative measures
A source of comfort in the midst of sorrow and loss is social support, whether it comes from peers or from one’s parents (Demazure et al., 2017). If the young people have foster parents or guardians in specific situations, it may be possible for them to express their feelings of despair and hopelessness more effectively. Given the fact that many of the UASCs have lost attachment figures and other members of their families, providing them with a family structure in a foster placement would aid them in re-establishing their sense of belonging and easing their transition into the local community. Even after they have settled into their new country, many immigrants will continue to be influenced by social turmoil and the fear of deportation that they have experienced on their journey. Socializing with those who come from similar backgrounds and, in certain cases, are of a similar age can help to ease depressive symptoms (Liebling et al., 2014). As a result of the group effect, UASCs are more likely than other children to benefit from the assistance provided by their caregivers. According to O’Higgins et al. (2018), there is a correlation between increased depressive symptoms and acculturative stress among UASCs who are placed in culturally matched foster households.
It is possible to reduce stress in children if they have a safe place to call home and can experience the warmth and compassion of an adult or caretaker who is concerned about them. Perhaps there is an association between the persistence of internalising symptoms and the stress that UASCs are subjected to (Vervliet, et al., 2014). According to various studies (Mels et al., 2008), there is a shortage of peer support, which highlights the need of caregivers or foster parents. Indeed, for those UASCs who are in regular contact with their families, this support serves as an antidote to stressful events that occur in their personal and professional life (Sierau, et al., 2018).
The ability to communicate mental health issues may be enhanced if UASCs have already made contact with MHS and are able to communicate their concerns. MHS exposure and symptoms of post-traumatic stress disorder (PTSD) were shown to be unrelated, whereas military service was found to be associated with symptoms of depression. Some speculate that this is related to referrers’ improved ability to define and recognise depression symptoms. The findings of the United Kingdom study were similar to those of the Dutch study in terms of unmet needs.
Despite the fact that the 2015–2016 European refugee crisis drew attention to this issue, screening and early detection of psychological distress among UASCs has remained a challenge (Fegert, et al., 2018). According to Goodman and Goodman (2012), self-report tools such as the Strengths and Difficulties Questionnaire (Goodman et al., 2000) used by social workers in the United Kingdom to assess UASCs may have insufficient sensitivity for diagnosing depression, anxiety disorders, and posttraumatic stress disorder (PTSD) in routine practise. As a result of improved screening, the most susceptible UASCs may be referred to specialists for appropriate care more promptly than previously.
It is possible that UASCs will be unwilling to accept support from adults, even if they are provided MHS, for a variety of reasons. Many of them would have gone through horrible situations in their home countries and on their journey, which were perpetrated by adults such as smugglers, traffickers, and customs officials. They may have difficulty placing their faith in someone they do not know. Another factor that may prevent people from seeking and receiving treatment from MHS is the fear of jeopardising their prospects of receiving sanctuary. Traumatic stress disorder (PTSD) is thought to be associated with a fear of disclosure, which could explain part of the avoidance that persons who suffer from PTSD display.
Because of language and cultural difficulties, UASCs from countries with little or no MHS service may be unaware that certain interventions and professionals, such as psychologists and therapists, are available to them in their home country. It is also conceivable that local children and adolescents are not aware of the services that are available to them, so even if they are distressed, they may not be able to express their distress or obtain the information essential to seek support from authorities.
Conclusion
When they arrive in their new countries, refugees and asylum seekers face a variety of challenges, such as “armed war, the loss or murder of family members, torture, arbitrary detention, and sexual and other types of abuse” Refugees frequently suffer from anxiety, depression, and post-traumatic stress disorder. According to prior systematic reviews, methodological inconsistencies, as well as individual characteristics and post-migratory pressures, account for much of the variation in prevalence rates. More than 20% of migrants are reported to suffer from anxiety, depression, or PTSD. Surveys on refugee children have found that the incidence of post-traumatic stress disorder (PTSD) ranges from 40% to 63%, while the prevalence of depression ranges from 25% to 50%. UASCs, on the other hand, necessitate extra care because to their increased susceptibility and the potential psychological harm they may suffer. The United Nations Refugee Agency (UNHCR) offers special care to children and adolescents because of their vulnerability. Protective measures, such as sufficient care and support, education, housing, and legal aid, must be provided by host countries to UASCs in order to assure their safety.
Due to the fact that they are not typically accompanied by their parents or other primary caretakers, UASCs are viewed as particularly vulnerable. Abuse, exploitation, and the loss of family members are all more likely to have affected them than unaccompanied minors and non-immigrants. Their scholastic and social lives are completely disturbed after surviving a series of traumatic experiences, including having their language skills and cultural acclimatisation challenged. Traumatic events in one’s life are associated with significant levels of psychological distress and an increased likelihood of developing a mental disorder. The UASC and their accompanying counterparts have not been compared to ascertain if the UASC had higher war trauma in their countries of origin.. It is possible to face additional dangers when travelling and arriving in resettlement countries. When individuals arrive in their new countries, the psychological tension caused by their previous challenges can be lessened. It’s unclear whether or not living in a supportive environment might lessen the effects of earlier trauma on a family’s ability to cope with separation. The fact that so many people in England are living alone and without any support makes this a crucial aspect of public mental health.
To answer these questions, the researchers set out to determine whether UASC had encountered more adversity and war trauma in the past and how these additional stresses may affect their mental health, as well as whether the UASC had higher levels of psychological distress. Based on the review of literature, the study has highlighted some intervention and preventative measures that could ease the transition and assimilation process for the UASCs.
References
Aliverti A (2012) Making people criminal: The role of the criminal law in immigration enforcement. Theoretical Criminology 16(4): 417–434. https://doi.org/10.1177/1362480612449779
All Party Parliamentary Group on Refugees (2017) Refugees Welcome? The Experience of New Refugees in the UK. London: AAPG. https://www.refugeecouncil.org.uk/assets/0004/0316/APPG_on_Refugees_-
Allsopp J, Sigona N and Phillimore J (2014) Poverty among refugees and asylum seekers in the UK: An evidence and policy review. IRiS Working Paper Series No. 1/2014. Edgbaston: University of Birmingham. https://www.birmingham.ac.uk/Documents/college-social-sciences/social-policy/iris/2014/working-paper- series/IRiS-WP-1-2014.pdf
Anderson J, Hollaus J, Lindsay A and Williamson C (2014) The culture of disbelief: An ethnographic approach to understanding an under-theorised concept in the UK asylum system. Working Paper Series No. 102. Oxford: Refugee Studies Centre. https://www.rsc.ox.ac.uk/files/files-1/wp102-culture-of-disbelief-2014.pdf
Behnia B (2015) Refugees’ convoy of social support. International Journal of Mental Health 32(4): 6–19. https://doi.org/10.1080/00207411.2003.11449595
Berry JW (2006) Acculturative stress. In Wong PTP and Wong LCJ (eds) Handbook of Multicultural Perspectives on Stress and Coping: 287–298. New York: Springer.
Bogic M, Njoku A, Priebe S. Long-term mental health of war- refugees: a systematic literature review. BMC Int Health Hum Rights. 2015;15(1):29.
Braun V and Clarke V (2006) Using thematic analysis in psychology. Qualitative Research in Psychology 3(2): 77–101. https://doi.org/10.1191/1478088706qp063oa
Bryman A (2008) Social Research Methods. 3rd ed. Oxford: Oxford University Press.
Butler J, Gambetti Z and Sabsay L (2016) Introduction. In Butler J, Gambetti Z and Sabsay L (eds) Vulnerability in Resistance. Durham: Duke University Press.
Cohen S (2001) States of Denial: Knowing About Atrocities and Suffering. Cambridge: Polity Press. Colman A (2015) A Dictionary of Psychology. 4th ed. Oxford: Oxford University Press.
Cohen, J., Mannarino, A. P., & Deblinger, E. (2006). Treating Trauma and Traumatic Grief in Children and Adolescents (1st Ed.). Guildford Press
Cortvriend, A. (2020). Coping with vulnerability: The Limbo created by the UK asylum system. In International Journal for Crime, Justice and Social Democracy (Vol. 9, Issue 3, pp. 61–74). Queensland University of Technology. https://doi.org/10.5204/ijcjsd.v9i3.1586
Crawley H, Hemmings J and Price N (2011) Coping with Destitution: Survival and Livelihood Strategies of Refused Asylum Seekers Living in the UK. Swansea: Centre for Migration Policy Research. https://policy- practice.oxfam.org.uk/publications/coping-with-destitution-survival-and-livelihood-strategies-of-refused- asylum-se-121667
Cuthill F, Siddiq Abdalla O and Bashir K (2013) Between Destitution and a Hard Place: Finding Strength to Survive Refusal from the Asylum System. Tyne and Wear: University of Sunderland. https://cityofsanctuary.org/wp- content/uploads/2015/02/cuthill_abdalla_and_bashir_2013between_destitution_and_a_hard_place_university_ of_sunderland_1.pdf
Demazure, G., Gaultier, S., & Pinsault, N. (2017). Dealing with difference: A scoping review of psychotherapeutic interventions with unaccompa- nied refugee minors. Journal of European Child and Adolescent Psychiatry [online], 27(4), 477–466. [Viewed 4 May 2018]. Available from: doi: https://doi.org/10.1007/s00787‐017‐1083‐y
Doggett CJ (2012) A Narrative Study of the Resilience and Coping of Unaccompanied Asylum-seeking Children and Young People (UASC) Arriving in a Rural Local Authority. PhD Thesis, University of Birmingham, United Kingdom.
El Baba, R., & Colucci, E. (2018). Post‐traumatic stress disorders, depres- sion, and anxiety in unaccompanied refugee minors exposed to war‐ related trauma: A systematic review. International Journal of Culture and Mental Health, 11(2), 194–207. https://doi.org/10.1080/17542863.2017.1355929
Fazel, M., Reed, R. V., Panter‐Brick, C., & Stein, A. (2011). Mental health of displaced and refugee children resettled in high‐income countries: Risk and protective factors. Lancet [online], 379(9812), 266–282. https://doi.org/10.1016/S0140‐ 6736(11)60051‐2
Fegert, J. M., Sukale, T., & Brown, R. C. (2018). Mental health service pro- vision for child and adolescent refugees: European perspectives. In M. Hodes, S. S.‐F. Gau, & P. J. de Vries (Eds.), Understanding uniqueness and diversity in child and adolescent mental health (pp. 193–220). London and San Diego: Academic Press.
Gadd D (2012) In-depth interviewing and psychosocial case study analysis. In Gadd D, Karstedt S and Messner SF (eds) The SAGE Handbook of Criminological Research Methods: 36–48. London: SAGE.
Gadeberg, A. K., Montgomery, E., Frederiksen, H. W., & Norredam, M. (2017). Assessing trauma and mental health in refugee children and youth: A systematic review of validated screening and measurement tools. European Journal of Public Health, 27(3), 439–446. https://doi. org/10.1093/eurpub/ckx034
Geltman, P., Grant‐Knight, W., Ellis, H., & Landgraf, J. M. (2008). The “lost boys” of Sudan: Use of health services and functional health outcomes of unaccompanied refugees minors resettled in the US. Journal of Immi- grant and Minority Health, 10(5), 389–396. https://doi.org/10.1007/ s10903‐007‐9110‐6
Geltman, P., Grant‐Knight, W., Mehta, S. D., Lloyd‐Travaglini, C., Lustig, S., Landgraf, J. M., & Wise, P. H. (2005). The “lost boys” of Sudan: Func- tional and behavioral health of unaccompanied refugees minors resettled in the US. Archives of Pediatrics and Adolescent Medicine, 159(6), 585–591. https://doi.org/10.1001/archpedi.159.6.585
Goodman, A., & Goodman, R. (2012). Strengths and difficulties question- naire scores and mental health in looked after children. The British Journal of Psychiatry: The Journal of Mental Science., 200(5), 426–427. https://doi.org/10.1192/bjp.bp.111.104380
Goodman, R., Ford, T., Simmons, H., Gatward, R., & Meltzer, H. (2000). Using the Strengths and Difficulties Questionnaire (SDQ) to screen for child psychiatric disorders in a community sample. The British Jour- nal of Psychiatry: The Journal of Mental Science., 177, 534–539. https:// doi.org/10.1192/bjp.177.6.534
Gower M (2016) Should asylum seekers have unrestricted rights to work in the UK? Commons Briefing Papers No.
Greenberg, M. T., & Riggs, N. R. (2015). Prevention of mental disorders and promotion of competence. In Rutter’s child and adolescent psychiatry (6th ed.). Oxford: Wiley‐Blackwell.
Healey R (2010) Gender variation in asylum experiences in the UK: The role of patriarchy and coping strategies.
Hodes, M., & Vostanis, P. (2018). Practitioner review: Mental health prob- lems of refugee children and adolescents and their management. Journal of Child Psychology and Psychiatry. https://doi.org/10.1111/ jcpp.13002
Hodes, M., Jagdev, D., Chandra, N., & Cunniff, A. (2008). Risk and resilience for psychological distress amongst unaccompanied asylum seeking adolescents. Journal of Child Psychology and Psychiatry and Allied Disciplines, 49(7), 723–732. https://doi.org/10.1111/j.1469-7610.2008.01912.x
Hodes, M., Jagdev, D., Chandra, N., & Cunniff, A. (2008). Risk and resil- ience for psychological distress amongst unaccompanied asylum seeking adolescents. Journal of Child Psychology and Psychiatry, 49(7), 723–732. https://doi.org/10.1111/j.1469‐7610.2008.01912.x
Hollway W and Jefferson T (2000) Doing Qualitative Research Differently. London: SAGE.
House of Commons Foreign Affairs Committee (2016) Libya: Examination of Intervention and Collapse and the UK’s Future Policy Options (HC 119). London: The Stationary Office. https://publications.parliament.uk/pa/cm201617/cmselect/cmfaff/119/119.pdf
House of Commons Home Affairs Committee (2017) Asylum Accommodation (HC 637). London: The Stationary Office. https://publications.parliament.uk/pa/cm201617/cmselect/cmhaff/637/637.pdf
International Organization for Migration (2019) IOM Libya 2017–2019: Migration Crisis Operational Framework.
International Organization for Migration (2020) Missing Migrants: Tracking Deaths Along Migratory Routes. https://missingmigrants.iom.int/region/europe
Jakobsen, M., Meyer DeMott, M. A., Wentzel‐Larsen, T., & Heir, T. (2017). The impact of the asylum process on mental health: A longitudinal study of unaccompanied refugee minors in Norway. BMJ Open [Online], 7, e015157. https://doi.org/10.1136/bmjopen‐2016‐015157
Johnson, F. M. (2020). Unaccompanied Asylum-Seeking Children: Childhood, Agency and Integration.
Journal of Identity and Migration Studies 4(2): 24–43.
Jubany O (2017) Screening Asylum in a Culture of Disbelief: Truths, Denials and Sceptical Borders. Basingstoke: Palgrave Macmillan.
Keles, S., Friborg, O., Idsoe, T., Sirin, S., & Oppedal, B. (2016). Depression among unaccompanied minor refugees: The relative contribution of general and acculturation‐specific daily hassles. Ethnicity & Health, 21(3), 300–317. https://doi.org/10.1080/13557858.2015.1065310
Keles, S., Friborg, O., Idsøe, T., Sirin, S., & Oppedal, B. (2018). Resilience and acculturation among unaccompanied refugee minors. International Journal of Behavioral Development, 42(1), 52–63. https://doi.org/10.1177/0165025416658136
Kronick, R. (2018). Mental Health of Refugees and Asylum Seekers: Assessment and Intervention. In Canadian Journal of Psychiatry (Vol. 63, Issue 5, pp. 290–296). SAGE Publications Inc. https://doi.org/10.1177/0706743717746665
Laban CJ (2015) Resilience-orientated treatment of traumatised asylum seekers and refugees. In Schouler-Ocak M (ed) Trauma and Migration: Cultural Factors in the Diagnosis and Treatment of Traumatised Immigrants: 191–
Laban CJ, Gernaat HB, Komproe IH, van der Tweel I and De Jong J (2005) Postmigration living problems and common psychiatric disorders in Iraqi asylum seekers in the Netherlands. Journal of Mental and Nervous Disease 193(12): 825–832. https://doi.org/10.1097/01.nmd.0000188977.44657.1d
Liebling H, Burke S, Goodman S and Zasada D (2014) Understanding the experiences of asylum seekers. Journal of Migration, Health and Social Care 10(4): 207–219. https://doi.org/10.1108/IJMHSC-06-2013-0016
Liebling, H., Burke, S., Goodman, S., & Zasada, D. (2014). Understanding the experiences of asylum seekers. International Journal of Migration, Health and Social Care, 10(4), 207–219. https://doi.org/10.1108/IJMHSC-06-2013-0016
Mels, C., Derluyn, I., & Broekaert, E. (2008). Social support in unaccompa- nied asylum‐seeking boys: A case study. Child: Care, Health and Development, 34(6), 757–762. https://doi.org/10.1111/j.1365‐ 2214.2008.00883.x
Michelson, D., & Sclare, I. (2009). Psychological needs, service utilization and provision of care in a specialist mental health clinic for young ref- ugees: A comparative study. Clinical Child Psychology and Psychiatry, 14(2), 273–296. https://doi.org/10.1177/1359104508100889
Mitra, R., & Hodes, M. (2019). Prevention of psychological distress and promotion of resilience amongst unaccompanied refugee minors in resettlement countries. In Child: Care, Health and Development (Vol. 45, Issue 2, pp. 198–215). Blackwell Publishing Ltd. https://doi.org/10.1111/cch.12640
Morina, N., Malek, M., Nickerson, A., & Bryant, R. A. (2017). Psychological interventions for post‐traumatic stress disorder and depression in young survivors in mass violence and low‐ and middle‐income coun- tries: Meta‐analysis. The British Journal of Psychiatry [online], 210(4), 247–254. https://doi.org/10.1192/bjp.bp.115.180265
O’Higgins, A., Ott, E. M., & Shea, M. W. (2018). What is the impact of placement type on educational and health outcomes of unaccompanied refugee minors? A systematic review of the evidence. Clinical Child and Family Psychology Review, 21, 1–12. https://doi.org/10.1007/s10567‐ 018‐0256‐7.
Oremus, M., Oremus, C., Hall, G. B., McKinnon, M. C., & ECT & Cognition Systematic Review Team (2012). Inter‐rater and test retest reliability of quality assessments by novice student raters using the Jadad and Newcastle‐Ottawa Scales. BMJ Open, 2(4), e001368. https://doi.org/ 10.1136/bmjopen‐2012‐001368
Oxfam and the Refugee Council (2002) Poverty and Asylum in the UK. London: Refugee Council. https://oxfamilibrary.openrepository.com/bitstream/handle/10546/112557/poverty-asylum-uk-010702- en.pdf?sequence=5
Pearl M and Zetter R (2001) From refuge to exclusion: Housing as an instrument of social exclusion for refugees and asylum seekers in the UK. In Somerville P, Bowes A, Robinson D and Steele A (eds) ‘Race’, Housing and Social Exclusion: 226–244. London: Jessica Kingsley.
Pemberton S (2015) Harmful Societies. Bristol: Bristol University Press.
Phillimore J, Ergun E, Goodson L and Hennessey D (2007) ‘They Do Not Understand the Problem I Have’: Refugee Well Being and Mental Health. Birmingham: University of Birmingham. https://lemosandcrane.co.uk/resources/JRF%20-
Reavell J, Fazil Q. The epidemiology of PTSD and depression in refugee minors who have resettled in developed countries. J Mental Health. 2017;26(1):74-83.
Reesp S (2003) Refuge or retrauma? The impact of asylum seeker status on the wellbeing of East Timorese women asylum seekers residing in the Australian community. Australasian Psychiatry 11(Suppl 1): S96–S101. https://doi.org/10.1046/j.1038-5282.2003.02022.x
Reijneveld, S., de Boer, J. B., Bean, T., & Korfker, D. G. (2005). Unaccompa- nied adolescents seeking asylum: Poorer mental health under a restrictive reception. The Journal of Nervous and Mental Disease, 193(11), 759–761. https://doi.org/10.1097/01.nmd.0000185870.
Renner W and Salem I (2009) Post-traumatic stress in asylum seekers and refugees from Chechnya, Afghanistan, and West Africa: Gender differences in symptomatology and coping. International Journal of Social Psychiatry 55(2): 99–108. https://doi.org/10.1177/0020764008092341
Rider E (2014) Asylum seekers’ credibility burden: Managing trauma in the asylum process without collective support. Journal of Sociology and Social Work 2(2): 263–284. https://doi.org/10.15640/jssw.v2n2a16
Sanchez‐Cao, E., Kramer, T., & Hodes, M. (2013). Psychological distress and mental health service contact of unaccompanied asylum‐seeking children. National Library of Medicine. Child: Care, Health and Develop- ment, 39(5), 651–659.
Schaefer J and Moos R (1998) The context for posttraumatic growth: Life crises, individual and social resources, and coping. In Tedeschi R, Park C and Calhoun L (eds) Posttraumatic Growth: Positive Changes in the Aftermath of Crisis: 99–126. Mahwah: Lawrence Erlbaum.
Schock K, Rosner R and Knaevelsrud C (2015) Impact of asylum interviews on the mental health of traumatized asylum seekers. European Journal of Psychotraumatology 6(1): 26286. https://doi.org/10.3402/ejpt.v6.26286
Schweitzer R, Greenslade J and Kagee A (2007) Coping and resilience in refugee from the Sudan: A narrative account. Australian and New Zealand Journal of Psychiatry 41(3): 282–288. https://doi.org/10.1080/00048670601172780
Sierau, S., Schneider, E., Nesterko, Y., & Glaesmer, H. (2018). Alone, but protected? Effects of social support on mental health of unaccompa- nied refugee minors. European Child & Adolescent Psychiatry, 1–12. https://doi.org/10.1007/s00787‐018‐1246‐5
Simich, L, Beiser M and Mawani FN (2003) Social support and the significance of shared experience in refugee migration and resettlement. Western Journal of Nursing Research 25(7): 872–891. https://doi.org/10.1177/0193945903256705
Sinnerbrink I, Silove D, Field A, Steel Z and Manicavasagar V (1997) Compounding of premigration trauma and postmigration stress in asylum seekers. Journal of Psychology 131(5): 463–470. https://doi.org/10.1080/00223989709603533
Skinner EA, Edge K, Altman J and Sherwood H (2003) Searching for the structure of coping: A review and critique of category systems for classifying ways of coping. Psychological Bulletin 129(2): 216–269. https://doi.org/10.1037/0033-2909.129.2.216
Slobodin O, de Jong JT. Mental health interventions for trau- matized asylum seekers and refugees: What do we know about their efficacy? Int J Soc Psychiatry. 2015;61(1):17-26.
Spasojevic J, Heffer RW and Snyder DK (2000) Effects of posttraumatic stress and acculturation on marital functioning in Bosnian refugee couples. Journal of Traumatic Stress 13(2): 205–217. https://doi.org/10.1023/A:1007750410122
Spicer N (2008) Places of exclusion and inclusion: Asylum-seeker and refugee experiences of neighbourhoods in the UK. Journal of Ethnic and Migration Studies 34(3): 491–510. https://doi.org/10.1080/13691830701880350
Tol, W. A., Song, S., & Jordans, M. J. D. (2013). Annual research review: Resilience and mental health in children and adolescents living in areas of armed conflict—A systematic review of findings in low‐ and middle‐ income countries. Journal of Child Psychology and Psychiatry [online], 54(4), 445–460. https://doi.org/10.1111/jcpp.12053
Tol, W. A., Song, S., & Jordans, M. J. D. (2013). Annual research review: Resilience and mental health in children and adolescents living in areas of armed conflict—A systematic review of findings in low‐ and middle‐ income countries. Journal of Child Psychology and Psychiatry [online], 54(4), 445–460. https://doi.org/10.1111/jcpp.12053
Tripoli: International Organization for Migration. https://www.iom.int/sites/default/files/our_work/DOE/MCOF/MCOF-Libya-2017-2019.pdf
Turrini G, Purgato M, Ballette F, Nose M, Ostuzzi G, Barbui C. (2017). Common mental disorders in asylum seekers and refugees: Umbrella review of prevalence and intervention studies. Int J Ment Health Syst., 11(51).
UK Home Office (2015) Asylum Policy Instruction: Assessing Credibility and Refugee Status. London: UK Home Office. https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/397778/ASSESSING_CREDI BILITY_AND_REFUGEE_STATUS_V9_0.pdf
UK Home Office (2019) Immigration Statistics, Year Ending December 2018: Data Tables. https://www.gov.uk/government/statistics/immigration-statistics-year-ending-december-2018-data-tables
UNHCR (2018). United Nations Refugee Agency—The Website, http://www.unhcr.org/uk/figures‐at‐a‐ glance.htmlx
UNICEF 2021. Child displacement. https://data.unicef.org/topic/child-migration-and-displacement/displacement/
United Nations Development Programme (2010) Human Development Report 2010: The Real Wealth of Nations— Pathways to Human Development, 20th Anniversary Edition. New York: UNDP. https://doi.org/10.18356/e5a0500a-en
Unterhitzenberger, J., Eberle‐Sejari, R., Rassenhofer, M., Sukale, T., Rosner, R., & Goldbeck, L. (2015). Trauma‐focused cognitive behavioral therapy with unaccompanied refugee minors; a case series. BMC Psychiatry [online], 15(260). [Viewed 11 August 2016] Available from:
Ward T and Maruna S (2007) Rehabilitation. London: Routledge.
Watts MJ and Bohle HG (1993) The space of vulnerability: The causal structure of hunger and famine. Progress in Human Geography 17(1): 43–67. https://doi.org/10.1177/030913259301700103
Webber L (2004) The war on migration. In Hillyard P, Pantazis C, Tombs S and Gordon D (eds) Beyond Criminology: Taking Harm Seriously: 133–155. London: Pluto Press.
Wells, G., Shea, B., O’Connell, D., Peterson, J., Welch, V., Losos, M., & Tugwell, P. (2018). The Newcastle‐Ottawa Scale (NOS) for assessing the quality of non‐randomised studies in meta‐analyses. In Ottawa hospital research institute.
Zwi, K., Mares, S., Nathanson, D., Tay, A. K., & Silove, D. (2018). The impact of detention on the social‐emotional wellbeing of children seeking asy- lum: A comparison with community‐based children. European Child & Adolescent Psychiatry, 27(4), 411–422.
………………………………………………………………………………………………………………………..
Know more about UniqueSubmission’s other writing services:


Thank you very much for sharing, I learned a lot from your article. Very cool. Thanks. nimabi